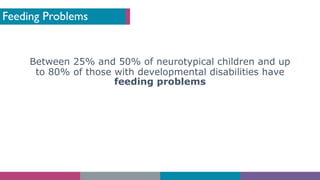
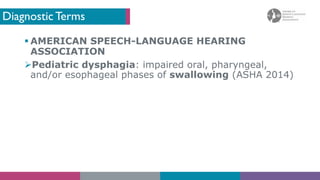
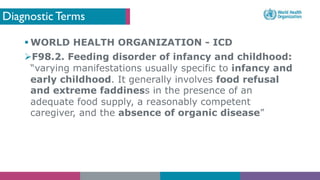
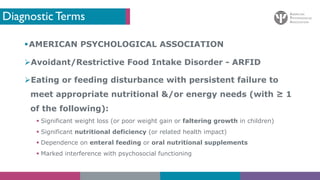
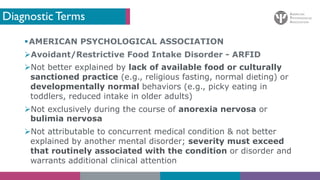
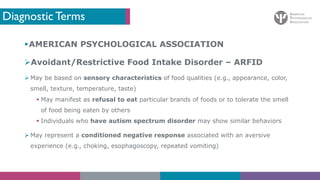
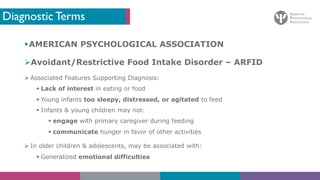
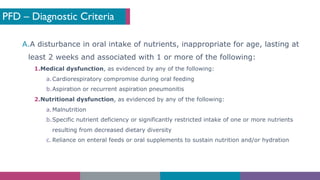
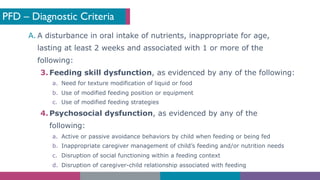
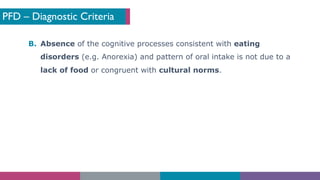
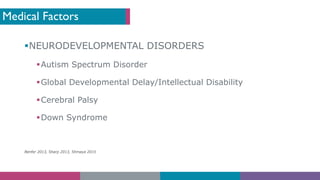
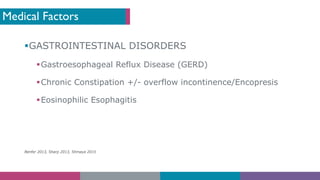
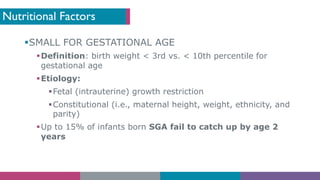
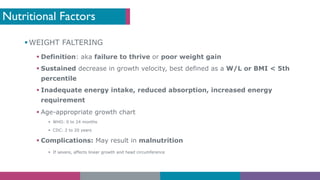
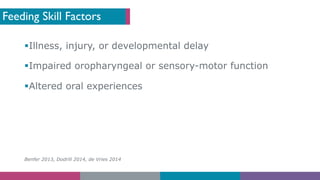
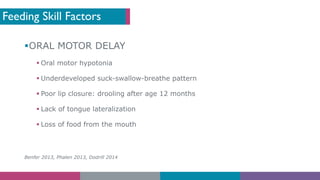
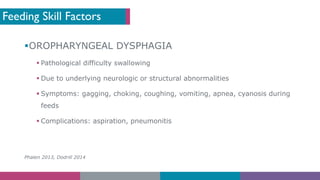
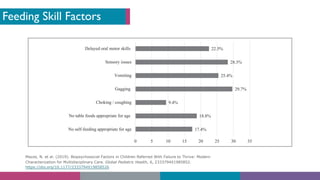
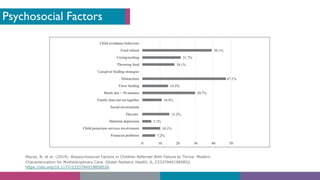
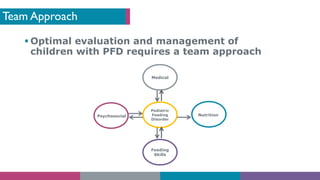
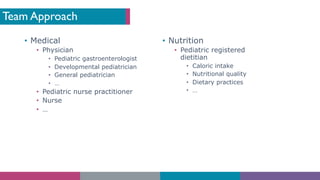
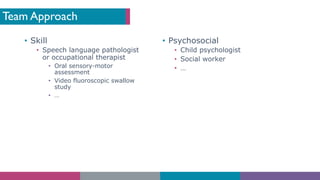
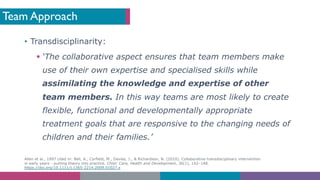
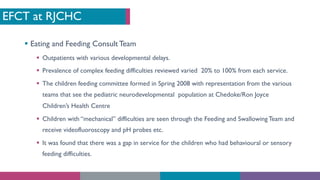
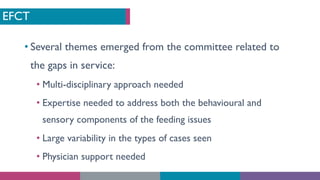
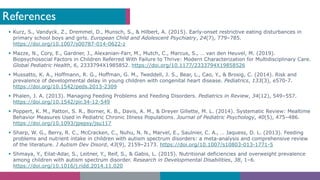
The document discusses pediatric feeding disorder (PFD), highlighting its lack of a universally accepted definition and the need for a unifying diagnostic term that encompasses medical, nutritional, feeding skill, and psychosocial concerns. It outlines diagnostic criteria for PFD, its associated factors including medical, nutritional, and psychosocial elements, and emphasizes the importance of a multidisciplinary team approach for effective management. The content includes references to various psychological and nutritional factors, as well as recommendations for treatment practices.