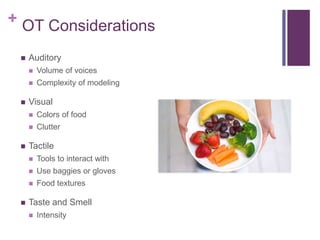
This document discusses feeding issues in pediatric occupational therapy. It notes that 20% of children struggle with feeding issues in their first 5 years, and 5-10% require medical intervention. Feeding issues are often mixed, involving both behavioral and organic components. Poor feeding can disrupt parent-child interactions and increase parental stress. Occupational therapy aims to establish mealtime routines, reduce food refusal through desensitization, and teach social skills modeling. Sensory-based strategies and multidisciplinary support can help address feeding challenges.