Avoidant/Restrictive Food Intake Disorder (ARFID) is a feeding disorder characterized by avoidance of food due to sensory characteristics, fear of aversive consequences, or lack of interest in eating. This results in insufficient calorie or nutrient intake leading to issues like weight loss, nutritional deficiencies, or interference with functioning. Treatments that have shown promise for ARFID include family-based treatment involving parents supporting exposure to new foods, cognitive-behavioral therapy with elements like food exposure and relaxation training, and hospital-based refeeding programs, some of which utilize tube feeding for severe cases. However, more research is still needed, as existing studies on treating ARFID are limited and no single approach has been proven


![Avoidant/restrictive food intake disorder; ARFID; family-based
treatment; cognitive-behavioral
therapy; tube feeding
Correspondence to: Jennifer J. Thomas, Ph.D., Eating Disorders
Clinical and Research Program, Massachusetts General
Hospital, 2
Longfellow Place, Suite 200, Boston, MA 02114.
[email protected] Phone: (617) 643-6306.
Conflicts of interest. Drs. Thomas and Eddy will receive
royalties from Cambridge University Press for the sale of their
book
Cognitive-Behavioral Therapy for Avoidant/Restrictive Food
Intake Disorder: Children, Adolescents, and Adults, scheduled
to be
published in late 2018.
HHS Public Access
Author manuscript
Curr Opin Psychiatry. Author manuscript; available in PMC
2019 November 01.
Published in final edited form as:
Curr Opin Psychiatry. 2018 November ; 31(6): 425–430.
doi:10.1097/YCO.0000000000000454.
A
u
th
o
r M
a
n](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-6-320.jpg)
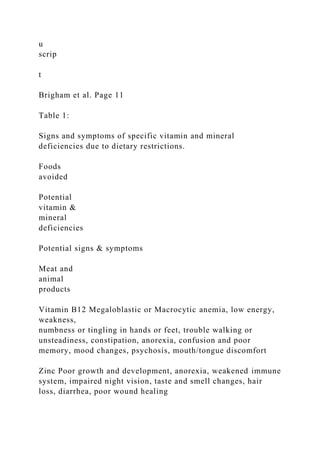
![o
r M
a
n
u
scrip
t
Introduction
Avoidant/restrictive food intake disorder (ARFID) made its
diagnostic debut in 2013 with
the publication on DSM-5 [1]. ARFID is a reformulation and
expansion of the former DSM-
IV diagnosis of feeding disorder of infancy and early childhood,
and can occur across the
lifespan. The hallmark feature of ARIFD is food avoidance or
restriction, motivated by
sensitivity to the sensory characteristics of food, fear of
aversive consequences of eating, or
lack of interest in eating or food. To meet criteria for ARFID,
the food restriction or
avoidance must lead to one or more consequences such as
weight loss or faltering growth,
nutritional deficiency, dependence on oral nutritional
supplements or tube feeding, or](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-8-320.jpg)
![psychosocial impairment. DSM-5 describes three example
presentations of ARFID. In the
first, individuals eat a very limited range of foods due to an
inability to tolerate certain tastes
and textures. In the second, individuals avoid specific foods or
categories of food, or may
stop eating altogether, for fear of aversive consequences of
eating, such as choking,
vomiting, anaphylaxis, or gastrointestinal distress. In the third,
individuals exhibit a lack of
interest in food or eating. It is important to note that these three
presentations are not
mutually exclusive and can co-occur within the same individual
[2].
In addition to the heterogeneity of clinical presentation, ARFID
is also quite diverse in terms
of age, demographics, and comorbidities, highlighting the
difficulty in identifying a
universally applicable treatment approach. For example, ARFID
has been reported in very
young children [3 **], adolescents [4 *], and adults [5], and
several studies have highlighted
that both males and females present with the disorder [6,7].
Other investigations have](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-9-320.jpg)
![underscored numerous potential psychiatric and medical
comorbidities, including autism
spectrum disorder [8] and gastrointestinal disorders [6], which
may further individualize
treatment needs.
Available data on the treatment of ARFID
Because ARFID is so new, there is currently no evidence-based
treatment suitable for all
forms of the disorder. A robust literature that pre-dates DSM-5
supports the efficacy of
behavioral interventions for young children with pediatric
feeding disorders [9,10].
However, the generalizability of these approaches to individuals
with ARFID—especially
adolescents and adults—remains unclear. Below we summarize
studies published since the
2013 advent of DSM-5 that describe the treatment of ARFID
specifically. ARFID treatments
recently described in the literature include family-based
treatment and parent training;
cognitive-behavioral approaches; hospital-based re-feeding
including tube feeding; and
adjunctive pharmacotherapy.
Family-based treatment and parent training](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-10-320.jpg)
![Several recently published case reports have described the use
of family-based treatment
(FBT) for children and adolescents with ARFID [11,12,13].
Such approaches are similar to
FBT for anorexia nervosa (AN) in that parents are charged with
the task of feeding, but
differ from FBT for AN in that parents are asked to support
their children in increasing not
only dietary volume, but also dietary variety through repeated
exposure to novel foods. At
least two clinical trials of FBT for ARFID are currently
underway [14,15]. Another case
Thomas et al. Page 2
Curr Opin Psychiatry. Author manuscript; available in PMC
2019 November 01.
A
u
th
o
r M
a
n
u
scrip
t](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-11-320.jpg)
![a
n
u
scrip
t
report described the use of a behavioral parent-training
intervention comprising differential
reinforcement, gradual exposure to novel foods, and
contingency management, resulting in
the acceptance of 30 novel foods in a six-year-old with limited
dietary variety [16].
Cognitive-behavioral approaches
Multiple published case reports and case series have described
the use of various forms of
cognitive-behavioral therapy (CBT) for children [13,17,18] and
adults [19,5] with ARFID.
Common elements across CBT interventions for ARFID include
regular eating [5,13], self-
monitoring of food intake [5], exposure and response prevention
[13,16], relaxation training
[17,16, and behavioral experiments [5]. In one case study, a 16-
year-old boy was able to
significantly increase his consumption of proteins, fruits, and](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-13-320.jpg)
![vegetables, and significantly
decrease his eating-related distress after 11 sessions of CBT
supplemented with in-home
meal interventions in which his mother reinforced the
consumption of novel foods [16].
Hospital-based re-feeding including tube feeding
Several hospital-based re-feeding programs have reported
positive outcomes on eating and
weight for children and adolescents with low-weight ARFID.
One randomized controlled
study prospectively evaluated the efficacy, among 20 boys and
girls (ages 13–72 months)
with ARFID, of a five-day manualized behavioral treatment
comprising structured
mealtimes, escape extinction, and reinforcement procedures in a
day hospital setting.
Patients randomized to the study treatment exhibited
significantly greater bite acceptance,
grams of food consumed at mealtime, and fewer mealtime
disruptions post-treatment
compared to those in the wait list control condition 3 **].
Another study described treatment
response among 32 children and adolescents with ARFID
treated in an eating disorders](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-14-320.jpg)
![partial hospitalization program, reporting significant increases
in weight and significant
decreases in eating pathology and anxiety from pre- to post-
treatment after an average of
seven weeks [4 *]. Treatment gains were maintained for at least
12 months in the subset of
20 patients who completed a follow-up assessment [20].
Several case studies have described the use of tube feeding to
support inpatient nutritional
rehabilitation among low-weight children and adolescents (ages
5–17 years old) with
ARFID [21,22,23]. Of note, at least two studies have reported
that patients with ARFID
were significantly more likely than those with other eating
disorders to require tube feeding
during inpatient hospitalization [24,25 *]. Although tube
feeding can be a life-saving
measure in some cases of acute food refusal, a recent review
described potentially iatrogenic
effects of tube feeding, including long-term tube dependence
and decreased oral intake [26],
highlighting the urgent need for future research on effective
tube weaning protocols for](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-15-320.jpg)
![individuals who require tube feeding.
Adjunctive pharmacotherapy
Three groups have recently published studies on
pharmacotherapy as an adjunct to hospital-
based treatment to facilitate meal consumption and/or weight
gain in low-weight children
and adolescents with ARFID. In one retrospective chart review,
14 children and adolescents
demonstrated a significantly faster rate of weight gain after
(versus before) being prescribed
mirtazapine [27 *]. In another retrospective chart review, nine
youth who took olanzapine
Thomas et al. Page 3
Curr Opin Psychiatry. Author manuscript; available in PMC
2019 November 01.
A
u
th
o
r M
a
n
u
scrip](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-16-320.jpg)
![a
n
u
scrip
t
showed significant increases in weight from pre- to post-
treatment [28 *]. The only double-
blind randomized placebo-controlled trial of medication for
ARFID evaluated the efficacy of
D-cycloserine (DCS) augmentation of a five-day behavioral
intervention for chronic and
severe food refusal in 15 children (ages 20–58 months). Those
randomized to the DCS
condition showed a significantly greater percentage of bites
rapidly swallowed, and
significantly fewer mealtime disruptions, compared to those
receiving placebo [29 **].
Summary of available data
Available data on the treatment of ARFID are sparse, and
limited to child and adolescent
populations. Studies are limited to case reports, case series, and
retrospective chart reviews,](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-18-320.jpg)
![with a handful of randomized controlled trials in very young
children treated in day hospital
settings. Findings in adults are limited to case reports, with no
larger-scale studies on
patients over the age of 18. Several groups are currently
evaluating the efficacy of new
psychological treatments for ARFID [14,15,30], but results have
not yet been published.
Case reports and case series have highlighted the promise of
family-based treatment,
cognitive-behavioral therapy, and hospital-based re-feeding,
with pharmacotherapy as an
adjunctive rather than a stand-alone treatment. Prospective
randomized controlled trials are
needed, particularly for adolescents and adults.
The cognitive-behavioral formulation of ARFID
To fill the need for manualized treatments suitable for testing in
randomized controlled
trials, our team at Massachusetts General Hospital has
developed a novel form of cognitive-
behavioral therapy for ARFID that is currently being tested in
an open trial in which 20
participants ages 10–22 are receiving either individual of
family-based versions of the](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-19-320.jpg)
![treatment [30,31 **]. The goal of CBT-AR is to help patients
achieve a healthy weight,
resolve nutrition deficiencies, increase variety to include
multiple foods from each of the
five basic food groups, eliminate dependence on nutritional
supplements, and reduce
psychosocial impairment. CBT-AR is based on our cognitive-
behavioral conceptualization
of the disorder (Figure 1), which posits that some individuals
have a biological
predisposition to sensory sensitivity, fear of aversive
consequences, and/or lack of interest in
food or eating [2]. Specifically, those with sensory sensitivity
may have heightened response
to unfamiliar tastes and smells, those with fear of aversive
consequences may have high trait
anxiety, and those with lack of interest in eating or food may
have lower homeostatic or
hedonic appetites.
The CBT model posits that individuals with such
predispositions will be vulnerable to
developing negative feelings and predictions about eating. For
example, the patient with](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-20-320.jpg)
![children, adolescents, and adults with ARFID (ages 10 and up).
CBT-AR is a flexible,
modular treatment designed to last approximately 20 (for
patients who are not underweight)
to 30 (for patients who have significant weight to gain) sessions
over six to 12 months. CBT-
AR is appropriate for individuals with ARFID who are
medically stable, currently accepting
at least some food by mouth, and not receiving tube feeding.
Patients who are under the age
of 16 and/or older adolescents and young adult patients who
have significant weight to gain
can be offered a family-supported version of CBT-AR, whereas
patients ages 16 years and
up without significant weight to gain can be treated with an
individual version.
CBT-AR proceeds through four broad stages (Table 1) [31 **].
In Stage 1, the therapist
provides psychoeducation about ARFID and CBT-AR. In
addition, the therapist encourages
the patient to establish a pattern of regular eating and self-
monitoring by relying primarily
on preferred foods, but also encourages early change by asking
the patient who is not](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-24-320.jpg)
![clinical needs.
Acknowledgments
Disclosure of funding. The authors would like to gratefully
acknowledge funding for the work described in this
paper from the National Institute of Mental Health
(1R01MH108595), Hilda and Preston Davis Foundation, and
American Psychological Foundation.
References and Recommended Reading
Papers of particular interest, published within the annual period
of review, have been
highlighted as:
* of special interest
** of outstanding interest
1. American Psychiatric Association. Diagnostic and statistical
manual of mental disorders (DSM-5).
American Psychiatric Pub; 2013.
2. Thomas JJ, Lawson EA, Micali N et al. Avoidant/restrictive
food intake disorder: a three-
dimensional model of neurobiology with implications for
etiology and treatment. Current psychiatry
reports. 2017; 19:54. [PubMed: 28714048]
3 **. Sharp WG, Stubbs KH, Adams H et al. Intensive, manual-
based intervention for pediatric feeding
disorders: results from a randomized pilot trial. Journal of
pediatric gastroenterology and
nutrition. 2016; 62:658–63.](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-30-320.jpg)
![t
A
u
th
o
r M
a
n
u
scrip
t
A
u
th
o
r M
a
n
u
scrip
t
[PubMed: 26628445]
4 *. Ornstein RM, Essayli JH, Nicely TA et al. Treatment of
avoidant/restrictive food intake disorder in](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-32-320.jpg)
![a cohort of young patients in a partial hospitalization program
for eating disorders. International
Journal of Eating Disorders. 2017; 50:1067–74.
This retrospective chart review describes outcomes for children
and adolescents with ARFID treated in
a partial hospitalization program for eating disorders, which
utilizes techniques from family-
based treatment and cognitive-behavioral therapy.
[PubMed: 28644568]
5. Steen E, Wade TD. Treatment of co‐occurring food avoidance
and alcohol use disorder in an adult:
possible avoidant restrictive food intake disorder?. International
Journal of Eating Disorders. 2018;
51:373–377. [PubMed: 29394459]
6. Eddy KT, Thomas JJ, Hastings E et al. Prevalence of DSM‐5
avoidant/restrictive food intake
disorder in a pediatric gastroenterology healthcare network.
International Journal of Eating
Disorders. 2015; 48:464–70. [PubMed: 25142784]
7. Forman SF, McKenzie N, Hehn R et al. Predictors of outcome
at 1 year in adolescents with DSM-5
restrictive eating disorders: report of the national eating
disorders quality improvement
collaborative. Journal of Adolescent Health. 2014; 55:750–6.
[PubMed: 25200345]
8. Lucarelli J, Pappas D, Welchons L, Augustyn M. Autism
spectrum disorder and avoidant/restrictive
food intake disorder. Journal of Developmental & Behavioral](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-33-320.jpg)
![Pediatrics. 2017; 38:79–80. [PubMed:
27824638]
9. Lukens CT, Silverman AH. Systematic review of
psychological interventions for pediatric feeding
problems. Journal of pediatric psychology. 2014 6
13;39(8):903–17. [PubMed: 24934248]
10. Sharp WG, Volkert VM, Scahill L et al. A systematic review
and meta-analysis of intensive
multidisciplinary intervention for pediatric feeding disorders:
how standard is the standard of
care?. The Journal of pediatrics. 2017; 181:116–24. [PubMed:
27843007]
11. Fitzpatrick KK, Forsberg SE, Colborn. Family-based
therapy for avoidant restrictive food intake
disorder: Families Facing Food Neophobias In: Family Therapy
for Adolescent Eating and Weight
Disorders. 1 Loeb K. (Ed.), Le Grange D. (Ed.), Lock J. (Ed.).
New York: Routledge; 2015 pp.
276–296
12. Norris ML, Spettigue WJ, Katzman DK. Update on eating
disorders: current perspectives on
avoidant/restrictive food intake disorder in children and youth.
Neuropsychiatric disease and
treatment. 2016; 12:213–218. [PubMed: 26855577]
13. Thomas JJ, Brigham KS, Sally ST et al. Case 18–2017—an
11-year-old girl with difficulty eating
after a choking incident. New England journal of medicine.
2017; 376:2377–86. [PubMed:
28614676]
14. Lesser J, Eckhardt S, Ehrenreich-May J, et al. Integrating](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-34-320.jpg)
![family based treatment with the unified
protocol for the transdiagnostic treatment of emotional 351
disorders: a novel treatment for
avoidant restrictive food intake disorder. Clinical Teaching Day
presentation at the International
Conference on Eating Disorders; 2017; Prague, Czech Republic.
15. Sadeh-Sharvit S, Robinson A, Lock J. FBT-ARFID for
younger patients: lessons from a
randomized controlled trial. Workshop presented at the
International Conference on Eating
Disorders; 2018; Chicago, Illinois.
16. Murphy J, Zlomke KR. A behavioral parent-training
intervention for a child with avoidant/
restrictive food intake disorder. Clinical Practice in Pediatric
Psychology. 2016; 4:23–34.
17. Fischer AJ, Luiselli JK, Dove MB. Effects of clinic and in-
home treatment on consumption and
feeding-associated anxiety in an adolescent with
avoidant/restrictive food intake disorder. Clinical
Practice in Pediatric Psychology. 2015; 3:154–166.
18. Bryant Waugh R Avoidant restrictive food intake disorder:
an illustrative case example.
International Journal of Eating Disorders. 2013; 46:420–3.
[PubMed: 23658083]
19. King LA, Urbach JR, Stewart KE. Illness anxiety and
avoidant/restrictive food intake disorder:
cognitive-behavioral conceptualization and treatment. Eating
behaviors. 2015; 19:106–9.
[PubMed: 26276708]
Thomas et al. Page 7](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-35-320.jpg)
![o
r M
a
n
u
scrip
t
A
u
th
o
r M
a
n
u
scrip
t
20. Bryson AE, Scipioni AM, Essayli JH et al. Outcomes of
low‐weight patients with avoidant/
restrictive food intake disorder and anorexia nervosa at
long‐term follow‐up after treatment in a
partial hospitalization program for eating disorders.
International Journal of Eating Disorders.
2018; 51:470–474. [PubMed: 29493804]
21. Guvenek-Cokol PE, Gallagher K, Samsel C. Medical
traumatic stress: a multidisciplinary approach](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-37-320.jpg)
![for iatrogenic acute food refusal in the inpatient setting.
Hospital pediatrics. 2016; 6:693–8.
[PubMed: 27803075]
22. Pitt PD, Middleman AB. A focus on behavior management
of avoidant/restrictive food intake
disorder (ARFID): a case series. Clinical pediatrics. 2018;
57:478–80. [PubMed: 28719985]
23. Schermbrucker J, Kimber M, Johnson N et al.
Avoidant/restrictive food intake disorder in an 11-
year old south American boy: medical and cultural challenges.
Journal of the Canadian Academy
of Child and Adolescent Psychiatry. 2017; 26:110–113.
[PubMed: 28747934]
24. Strandjord SE, Sieke EH, Richmond M, Rome ES.
Avoidant/restrictive food intake disorder: illness
and hospital course in patients hospitalized for nutritional
insufficiency. Journal of Adolescent
Health. 2015; 57:673–8. [PubMed: 26422290]
25 *. Peebles R, Lesser A, Park CC et al. Outcomes of an
inpatient medical nutritional rehabilitation
protocol in children and adolescents with eating disorders.
Journal of eating disorders. 2017; 5:1–
14.
This paper describes the Children’s Hospital of Philadelphia
(CHOP) Malnutrition Protocol for the
inpatient re-feeding of children and adolescents with restrictive
eating disorders, including
ARFID.](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-38-320.jpg)
![[PubMed: 28053702]
26. Dovey TM, Wilken M, Martin CI, Meyer C. Definitions and
clinical guidance on the enteral
dependence component of the avoidant/restrictive food intake
disorder diagnostic criteria in
children. Journal of Parenteral and Enteral Nutrition. 2018;
42:499–507.
27 *. Gray E, Chen T, Menzel J et al. Mirtazapine and weight
gain in avoidant and restrictive food
intake disorder. Journal of the American Academy of Child &
Adolescent Psychiatry. 2018;
57:288–9.
This retrospective chart review describes adjuctive
pharmacotherapy with mirtazipine for children and
adolescents with ARFID.
[PubMed: 29588055]
28 *. Brewerton TD, D’Agostino M. Adjunctive use of
olanzapine in the treatment of avoidant
restrictive food intake disorder in children and adolescents in an
eating disorders program.
Journal of child and adolescent psychopharmacology. 2017;
27:920–2.
This retrospective chart review describes adjunctive
pharmacotherapy with olanazapine for children
and adolescents with ARFID.
[PubMed: 29068721]](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-39-320.jpg)



![papers have
addressed similar questions as those addressed in this article.
All study
procedures were approved by the University of Kansas
Institutional Re-
view Board (Study IRB STUDY00003260). Authors complied
with APA
ethical standards in the treatment of their participants. The
manuscript has
not been and is not posted on a website. Jenna P. Tregarthen is a
co-founder
and shareholder of Recovery Record, Inc. Jenna P. Tregarthen
made a
substantial contribution as part of data collection and curation
and ap-
proved the final manuscript, but she did not participate in the
analysis,
interpretation, or drafting of the manuscript. Kelsie T. Forbush
received an
industry-sponsored grant from Recovery Record, Inc. No other
authors
have conflicts of interest to disclose.
Correspondence concerning this article should be addressed to
Cheri A.
Levinson, Department of Psychological and Brain Sciences,
University of
Louisville, Life Sciences Building 317, Louisville, KY 40292.
E-mail:
[email protected]
T
hi
s
do](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-53-320.jpg)
![oa
dl
y.
Journal of Abnormal Psychology
© 2019 American Psychological Association 2020, Vol. 129,
No. 2, 177–190
ISSN: 0021-843X http://dx.doi.org/10.1037/abn0000477
177
https://orcid.org/0000-0001-7741-1498
mailto:[email protected]
http://dx.doi.org/10.1037/abn0000477
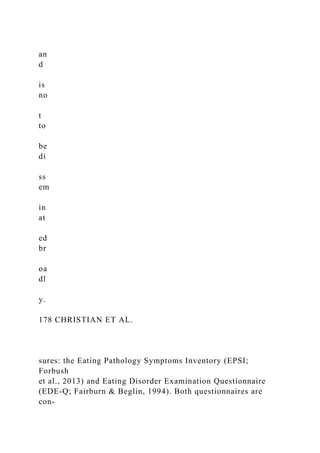
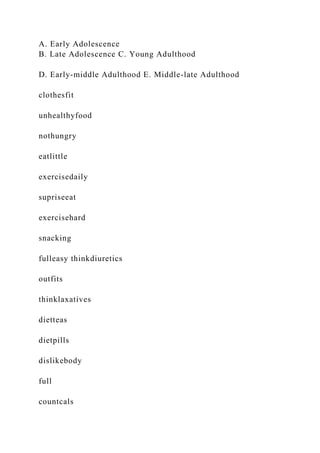
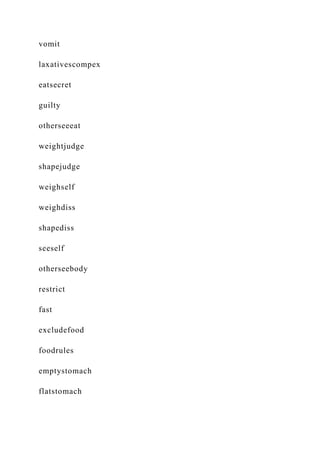
Eating disorders (EDs) are serious mental illnesses associated
with negative health consequences, significant impairment, and
high mortality (Crow et al., 2009; Rome & Ammerman, 2003;
Stice, Marti, & Rohde, 2013). Peak age of ED onset is during
adolescence, between 16 and 20 years of age (Stice et al.,
2013).
Although EDs most commonly develop during this period, evi-
dence suggests that eating pathology may persist, return, or de-
velop throughout an individual’s life (Fulton, 2016; Patrick &
Stahl, 2009). Indeed, studies indicate that ED symptoms occur
across all developmental stages, with approximately 11% of
adults
aged 42–55 and 4% of adults aged 60 –70 engaging in ED
behav-
iors, such as binge eating, laxative/diuretic misuse, or self-
induced
vomiting (Mangweth-Matzek et al., 2006; Marcus, Bromberger,
Wei, Brown, & Kravitz, 2007). The presence of disordered](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-58-320.jpg)



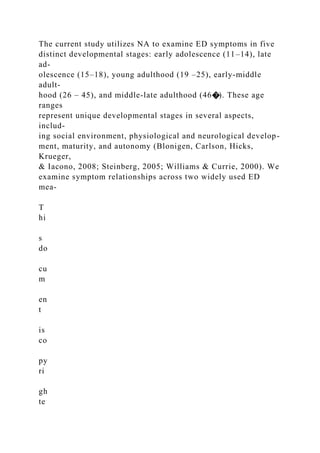

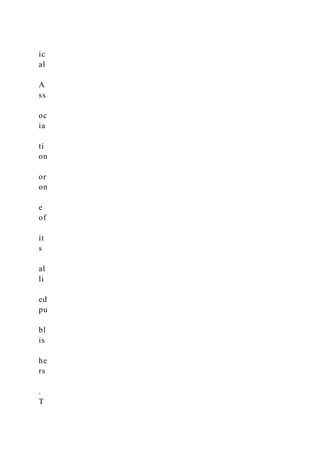
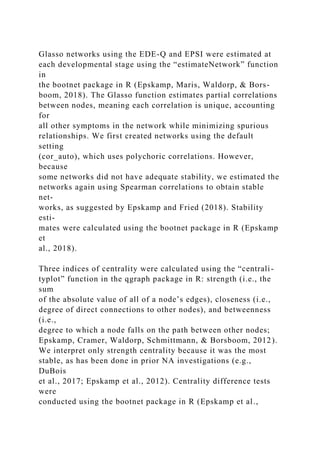
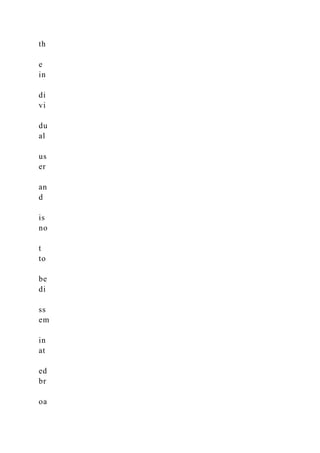
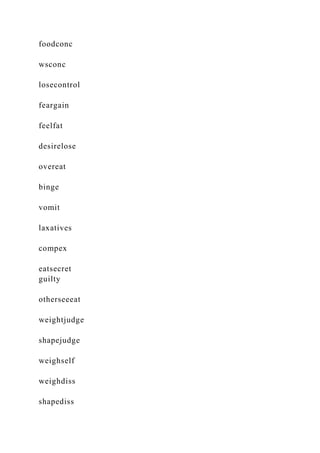
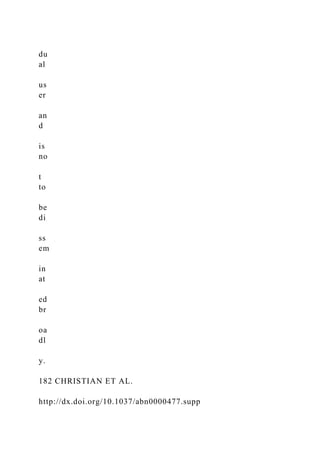
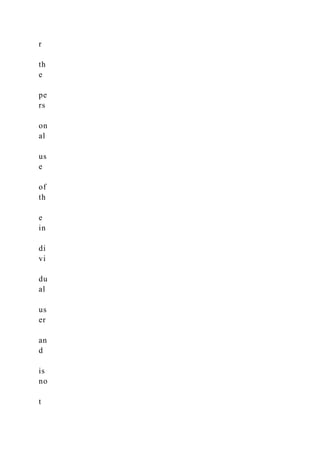
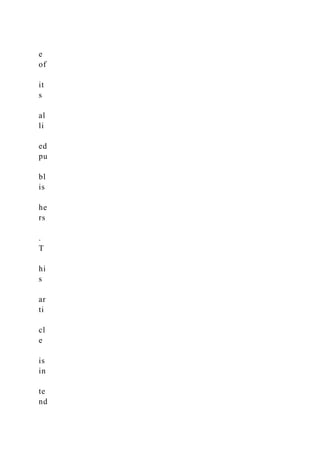
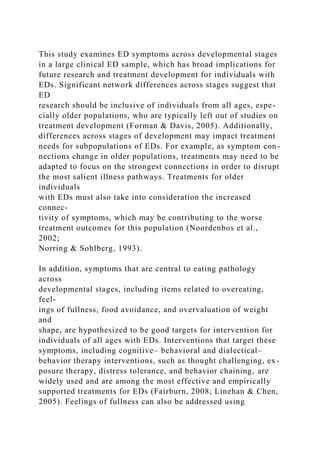
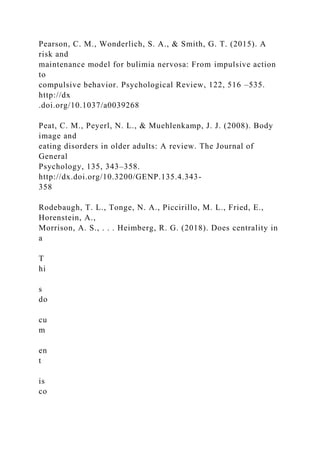
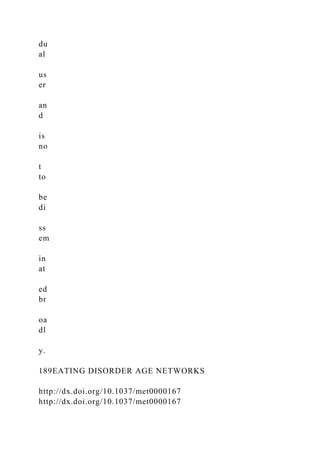
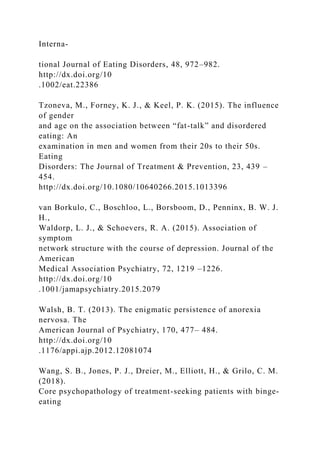
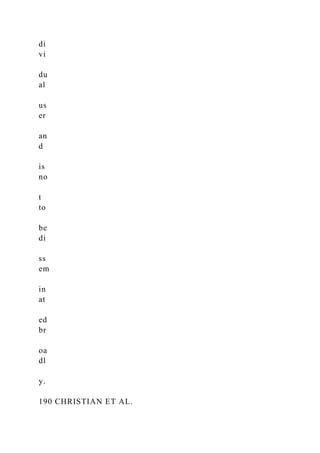
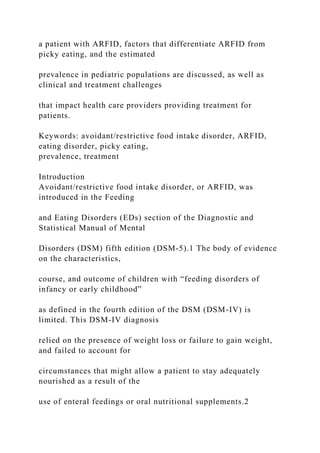
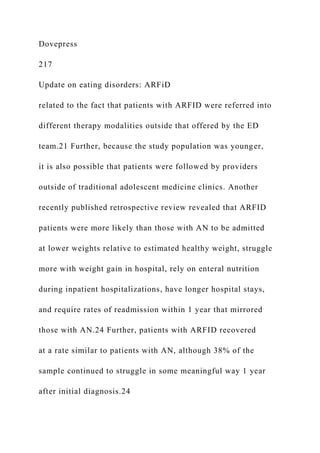
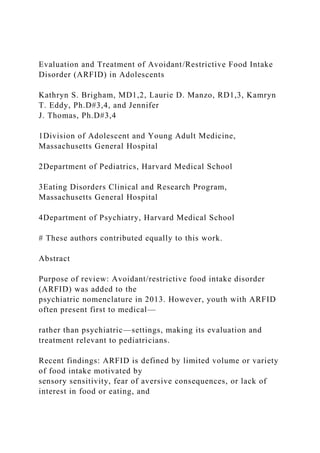
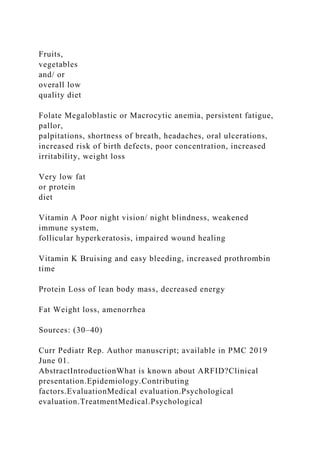
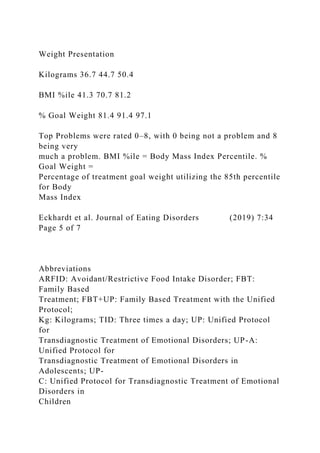
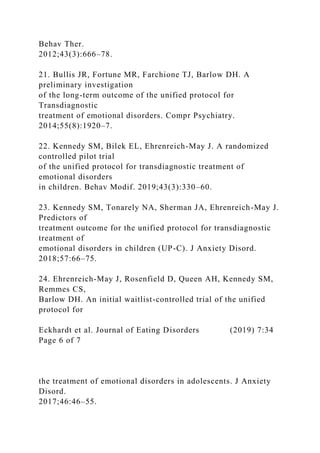
![AN 13 (.9) 85 (.9) 159 (1.4) 133 (1.7) 19 (1.6)
BN 2 (.1) 37 (.4) 99 (.8) 104 (1.3) 12 (1.0)
BED 4 (.3) 12 (.1) 49 (.4) 104 (1.3) 55 (4.6)
Other 3 (.2) 42 (.4) 93 (.8) 102 (1.3) 18 (1.5)
Missing 1501 (98.6) 9662 (98.2) 11309 (96.6) 7522 (94.6) 1090
(91.3)
Duration of illness (M[SD]) 1.71 (1.71) 2.92 (2.27) 5.82 (3.96)
13.86 (8.37) 29.00 (14.60)
EPSI 1028 (100) 6171 (100) 10701 (100) 9929 (100) 2073 (100)
Gender
Female 959 (93.3) 5786 (93.8) 10108 (94.5) 9412 (94.8) 1857
(89.6)
Male 46 (4.5) 228 (3.7) 381 (3.6) 438 (4.4) 201 (9.7)
Missing 23 (2.2) 157 (2.5) 212 (2.0) 79 (.8) 15 (.7)
Diagnosis
AN 152 (14.8) 796 (12.9) 1456 (13.6) 995 (10.0) 172 (8.3)
BN 30 (2.9) 307 (5.0) 870 (8.1) 825 (8.3) 81 (3.9)
BED 31 (3.0) 165 (2.7) 514 (4.8) 1144 (11.5) 527 (25.4)
Other 62 (6.0) 354 (5.7) 795 (7.4) 830 (8.4) 222 (10.7)
Missing 753 (73.2) 4549 (73.7) 7066 (66.0) 6134 (61.8) 1071
(51.7)
Duration of illness (M[SD]) 2.06 (2.11) 3.19 (2.44) 6.05 (4.12)
14.54 (8.58) 29.12 (15.20)
Note. EDE-Q � Eating Disorder Examination Questionnaire;
EPSI � Eating Pathology Symptoms Inventory; AN � anorexia
nervosa; BN � bulimia
nervosa; BED � binge eating disorder.
T
hi](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-71-320.jpg)
![ed
br
oa
dl
y.
179EATING DISORDER AGE NETWORKS
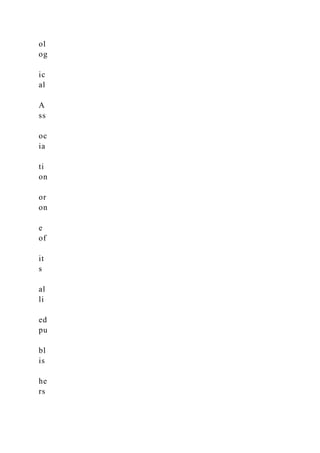
participants’ gender, ED diagnoses, and duration of illness
across
developmental categories.
Measures
EPSI. The EPSI is a 45-item multidimensional measure de-
signed to assess ED symptoms. The EPSI has eight scales corre-
sponding to unique facets of eating pathology: Body
Dissatisfac-
tion (i.e., satisfaction with body shape and body parts; e.g.,
hips,
thighs), Binge Eating (i.e., tendency to overeat or eat
mindlessly),
Cognitive Restraint (i.e., attempting to restrict eating, whether
successful or not), Excessive Exercise (i.e., intense or
compulsive
exercise), Restricting (i.e., efforts to avoid or reduce eating),
Purging (i.e., self-induced vomiting and laxative/diuretic use),
Muscle Building (i.e., cognitions and behaviors [supplement
use]
related to increasing muscularity), and Negative Attitudes
Toward
Obesity (i.e., negative judgment of individuals who are over-](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-76-320.jpg)




























![.1080/10640260590932841
Forrest, L. N., Jones, P. J., Ortiz, S. N., & Smith, A. R. (2018).
Core
psychopathology in anorexia nervosa and bulimia nervosa: A
network
analysis. International Journal of Eating Disorders, 51, 668 –
679. http://
dx.doi.org/10.1002/eat.22871
Fried, E. I., & Cramer, A. O. J. (2017). Moving forward:
Challenges and
directions for psychopathological network theory and
methodology.
Perspectives on Psychological Science, 12, 999 –1020.
http://dx.doi.org/
10.1177/1745691617705892
Fulton, C. L. (2016). Disordered eating across the lifespan of
women
[PDF]. Retrieved from https://www.counseling.org/docs/default-
source/
vistas/disordered-eating.pdf?sfvrsn�769e4a2c_4
Gadalla, T. M. (2008). Eating disorders and associated
psychiatric comor-
bidity in elderly Canadian women. Archives of Women’s Mental
Health,
11, 357–362. http://dx.doi.org/10.1007/s00737-008-0031-8
Goldschmidt, A. B., Crosby, R. D., Cao, L., Moessner, M.,
Forbush, K. T.,
Accurso, E. C., & Le Grange, D. (2018). Network analysis of
pediatric
eating disorder symptoms in a treatment-seeking,
transdiagnostic sam-](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-164-320.jpg)



![with AN as they lacked
Correspondence: Mark L Norris
Division of Adolescent Medicine,
Department of Pediatrics, Children’s
Hospital of eastern Ontario, University
of Ottawa, 401 Smyth Road, Ottawa,
ON K1H 8L1, Canada
Tel +1 613 737 7600
Fax +1 613 738 4878
email [email protected]
Journal name: Neuropsychiatric Disease and Treatment
Article Designation: Review
Year: 2016
Volume: 12
Running head verso: Norris et al
Running head recto: Update on eating disorders: ARFID
DOI: http://dx.doi.org/10.2147/NDT.S82538
http://www.dovepress.com/permissions.php
https://www.dovepress.com/terms.php
http://creativecommons.org/licenses/by-nc/3.0/
https://www.dovepress.com/terms.php
www.dovepress.com
www.dovepress.com
www.dovepress.com
http://dx.doi.org/10.2147/NDT.S82538
mailto:[email protected]
Neuropsychiatric Disease and Treatment 2016:12submit your
manuscript | www.dovepress.com
Dovepress
Dovepress](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-188-320.jpg)



![texture, taste, appearance); a fear
Corresponding author:Kathryn S. Brigham, MD, Division of
Adolescent and Young Adult Medicine, Massachusetts General
Hospital. 55 Fruit St- Yawkey 6D, Boston, MA 02114,
[email protected]
HHS Public Access
Author manuscript
Curr Pediatr Rep. Author manuscript; available in PMC 2019
June 01.
Published in final edited form as:
Curr Pediatr Rep. 2018 June ; 6(2): 107–113.
doi:10.1007/s40124-018-0162-y.
A
u
th
o
r M
a
n
u
scrip
t
A
u
th
o
r M](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-216-320.jpg)













![References
(1). American Psychiatric Association, American Psychiatric
Association DSM-5 Task Force.
Diagnostic and statistical manual of mental disorders : DSM-5.
5th ed. ed. Arlington, VA; 2013.
(2). American Psychiatric Association, American Psychiatric
Association Task Force on DSM.
Diagnostic and statistical manual of mental disorders : DSM-IV.
4th ed. ed. Washington, DC;
1994.
(3). Thomas JJ, Lawson EA, Micali N, Misra M, Deckersbach T,
Eddy KT. Avoidant/Restrictive Food
Intake Disorder: a Three-Dimensional Model of Neurobiology
with Implications for Etiology and
Treatment. Curr Psychiatry Rep 2017 8;19(8):54–017–0795–5.
[PubMed: 28714048]
(4). Fisher MM, Rosen DS, Ornstein RM, Mammel KA,
Katzman DK, Rome ES, et al. Characteristics
of avoidant/restrictive food intake disorder in children and
adolescents: a “new disorder” in
DSM-5. J Adolesc Health 2014 7;55(1):49–52. [PubMed:
24506978]
(5). Norris ML, Spettigue WJ, Katzman DK. Update on eating
disorders: current perspectives on
avoidant/restrictive food intake disorder in children and youth.
Neuropsychiatr Dis Treat 2016 1
19;12:213–218. [PubMed: 26855577]
(6). Eddy KT, Thomas JJ, Hastings E, Edkins K, Lamont E,
Nevins CM, et al. Prevalence of DSM-5
avoidant/restrictive food intake disorder in a pediatric](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-250-320.jpg)
![gastroenterology healthcare network. Int J
Eat Disord 2015 7;48(5):464–470. [PubMed: 25142784]
(7). Hay P, Mitchison D, Collado AEL, Gonzalez-Chica DA,
Stocks N, Touyz S. Burden and health-
related quality of life of eating disorders, including
Avoidant/Restrictive Food Intake Disorder
(ARFID), in the Australian population. J Eat Disord 2017 7
3;5:21-017-0149-z. eCollection
2017.
(8). Kurz S, van Dyck Z, Dremmel D, Munsch S, Hilbert A.
Early-onset restrictive eating disturbances
in primary school boys and girls. Eur Child Adolesc Psychiatry
2015 7;24(7):779–785. [PubMed:
25296563]
Brigham et al. Page 8
Curr Pediatr Rep. Author manuscript; available in PMC 2019
June 01.
A
u
th
o
r M
a
n
u
scrip
t
A](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-251-320.jpg)
![n
u
scrip
t
(9). Forman SF, McKenzie N, Hehn R, Monge MC, Kapphahn
CJ, Mammel KA, et al. Predictors of
outcome at 1 year in adolescents with DSM-5 restrictive eating
disorders: report of the national
eating disorders quality improvement collaborative. J Adolesc
Health 2014 12;55(6):750–756.
[PubMed: 25200345]
(10). Norris ML, Robinson A, Obeid N, Harrison M, Spettigue
W, Henderson K. Exploring avoidant/
restrictive food intake disorder in eating disordered patients: a
descriptive study. Int J Eat Disord
2014 ;47(5):495–499. [PubMed: 24343807]
(11). Ornstein RM, Rosen DS, Mammel KA, Callahan ST,
Forman S, Jay MS, et al. Distribution of
eating disorders in children and adolescents using the proposed
DSM-5 criteria for feeding and
eating disorders. J Adolesc Health 2013 ;53(2):303–305.
[PubMed: 23684215]
(12). Nicely TA, Lane-Loney S, Masciulli E, Hollenbeak CS,
Ornstein RM. Prevalence and
characteristics of avoidant/restrictive food intake disorder in a
cohort of young patients in day
treatment for eating disorders. J Eat Disord 2014 8 2;2(1):21-
014-0021-3. eCollection 2014.](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-253-320.jpg)
![(13). Ornstein RM, Essayli JH, Nicely TA, Masciulli E, Lane-
Loney S. Treatment of avoidant/
restrictive food intake disorder in a cohort of young patients in
a partial hospitalization program
for eating disorders. Int J Eat Disord 2017 9;50(9):1067–1074.
[PubMed: 28644568]
(14). Mammel KA, Ornstein RM. Avoidant/restrictive food
intake disorder: a new eating disorder
diagnosis in the diagnostic and statistical manual 5. Curr Opin
Pediatr 2017 8;29(4):407–413.
[PubMed: 28537947]
(15). Thomas JJ, Brigham KS, Sally ST, Hazen EP, Eddy KT.
Case 18-2017 - An 11-Year-Old Girl
with Difficulty Eating after a Choking Incident. N Engl J Med
2017 6 15;376(24):2377–2386.
[PubMed: 28614676]
(16). Marild K, Stordal K, Bulik CM, Rewers M, Ekbom A, Liu
E, et al. Celiac Disease and Anorexia
Nervosa: A Nationwide Study. Pediatrics 2017
5;139(5):10.1542/peds.2016-4367. Epub 2017
Apr 3.
(17). De Souza MJ, Nattiv A, Joy E, Misra M, Williams NI,
Mallinson RJ, et al. 2014 Female Athlete
Triad Coalition Consensus Statement on Treatment and Return
to Play of the Female Athlete
Triad: 1st International Conference held in San Francisco,
California, May 2012 and 2nd
International Conference held in Indianapolis, Indiana, May
2013. Br J Sports Med 2014 2;48(4):
289-2013-093218.
(18). Setnick J Micronutrient deficiencies and supplementation](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-254-320.jpg)
![in anorexia and bulimia nervosa: a
review of literature. Nutr Clin Pract 2010 ;25(2):137–142.
[PubMed: 20413694]
(19). Society for Adolescent Health and Medicine, Golden NH,
Katzman DK, Sawyer SM, Ornstein
RM, Rome ES, et al. Position Paper of the Society for
Adolescent Health and Medicine: medical
management of restrictive eating disorders in adolescents and
young adults. J Adolesc Health
2015 1;56(1):121–125. [PubMed: 25530605]
(20). Bryant-Waugh R, Micali N, Cooke L, et al. The Pica,
ARFID, and Rumination Disorder
Interview: Development of a multi-informant, semi-structured
interview of feeding disorders
across the lifespan. In preparation
(21). Hilbert A, van Dyck Z. Eating Disorders in Youth-
Questionnaire. English version . 2016 6 21;
Available at: http://nbn-resolving.de/urn:nbn:de:bsz:15-qucosa-
197246. Accessed Feb 28, 2018.
(22). Zickgraf HF, Ellis JM. Initial validation of the Nine Item
Avoidant/Restrictive Food Intake
disorder screen (NIAS): A measure of three restrictive eating
patterns. Appetite 2018 4 1;123:32–
42. [PubMed: 29208483]
(23). Strandjord SE, Sieke EH, Richmond M, Rome ES.
Avoidant/Restrictive Food Intake Disorder:
Illness and Hospital Course in Patients Hospitalized for
Nutritional Insufficiency. J Adolesc
Health 2015 12;57(6):673–678. [PubMed: 26422290]
(24). Brown J, Kim C, Lim A, Brown S, Desai H, Volker L, et](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-255-320.jpg)
![al. Successful gastrostomy tube weaning
program using an intensive multidisciplinary team approach. J
Pediatr Gastroenterol Nutr 2014
6;58(6):743–749. [PubMed: 24509305]
(25). Sharp WG, Stubbs KH, Adams H, Wells BM, Lesack RS,
Criado KK, et al. Intensive, Manual-
based Intervention for Pediatric Feeding Disorders: Results
From a Randomized Pilot Trial. J
Pediatr Gastroenterol Nutr 2016 4;62(4):658–663. [PubMed:
26628445]
Brigham et al. Page 9
Curr Pediatr Rep. Author manuscript; available in PMC 2019
June 01.
A
u
th
o
r M
a
n
u
scrip
t
A
u
th
o](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-256-320.jpg)
![http://nbn-resolving.de/urn:nbn:de:bsz:15-qucosa-197246
(26). Sant’Anna AM, Hammes PS, Porporino M, Martel C,
Zygmuntowicz C, Ramsay M. Use of
cyproheptadine in young children with feeding difficulties and
poor growth in a pediatric feeding
program. J Pediatr Gastroenterol Nutr 2014 11;59(5):674–678.
[PubMed: 24941960]
(27). Thomas J, Eddy K. Cognitive-behavioral therapy for
avoidant/restrictive food intake disorder:
Children, adolescents, and adults Cambridge, UK: Cambridge
University Press; In press 2018.
(28). Kardas M, Cermik BB, Ekmekci S, Uzuner S, Gokce S.
Lorazepam in the treatment of
posttraumatic feeding disorder. J Child Adolesc
Psychopharmacol 2014 6;24(5):296–297.
[PubMed: 24813692]
(29). Brewerton TD, D’Agostino M. Adjunctive Use of
Olanzapine in the Treatment of Avoidant
Restrictive Food Intake Disorder in Children and Adolescents in
an Eating Disorders Program. J
Child Adolesc Psychopharmacol 2017 12;27(10):920–922.
[PubMed: 29068721]
(30). Mueller C editor. The ASPEN Adult Nutrition Support
Core Curriculum 3rd ed. Silver Spring,
MD: American Society for Parenteral and Enteral Nutrition;
2017.
(31). Office of Dietary Supplements, National Institutes of
Health (US). Folate 2016 4 20; Available at:](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-258-320.jpg)
![UP for ARFID. Further research is needed to evaluate the use of
this treatment in patients presenting with a variety of
ARFID symptoms.
Keywords: Avoidant/restrictive food intake disorder, Emotional
disorders, Family-based treatment, Unified protocol,
Transdiagnostic
Background
Avoidant/Restrictive Food Intake Disorder (ARFID), a com-
plex and heterogeneous diagnosis, has been hypothesized
along a dimensional model with presentations including
sensory sensitivity, fear of aversive consequences, and lack
of interest in eating [1, 2]. Significant literature exists on
the treatment of pediatric feeding disorders supporting the
use of behavioral feeding interventions among young chil-
dren [3]. Recently, individual case reports/series have sug-
gested other promising approaches for older children,
adolescents, and adults with ARFID, using as a base either
family-based treatment (FBT) [4–7];, cognitive behavioral
therapy (CBT) [8–10];, or other novel approaches [11].
Despite these new approaches being studied, no published,
randomized controlled trials have yet to evaluate their effi-
cacy for the treatment of ARFID [2]. What appears to be
lacking in the current treatment models is the ability to
concurrently address the high rates of comorbid mood
and anxiety disorders in patients with ARFID [12, 13],
while also remaining focused on the medical complica-
tions associated with those patients who present under-
weight or exhibit significant nutritional deficiencies as
part of this diagnosis. Consequently, this case presentation
proposes a novel treatment approach that attempts to ad-
dress both the psychological and emotional comorbidities
associated in children and adolescents with ARFID, as well
as the hallmark food avoidance features that appear across](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-268-320.jpg)
![a heterogeneous array of presentations.
This case study describes the treatment of a patient
with ARFID, using a combined approach of FBT [14]
and the Unified Protocol for Transdiagnostic Treatment
of Emotional Disorders in Children (UP-C) [15]. FBT +
© The Author(s). 2019 Open Access This article is distributed
under the terms of the Creative Commons Attribution 4.0
International License
(http://creativecommons.org/licenses/by/4.0/), which permits
unrestricted use, distribution, and
reproduction in any medium, provided you give appropriate
credit to the original author(s) and the source, provide a link to
the Creative Commons license, and indicate if changes were
made. The Creative Commons Public Domain Dedication waiver
(http://creativecommons.org/publicdomain/zero/1.0/) applies to
the data made available in this article, unless otherwise stated.
* Correspondence: [email protected]
1Center for the Treatment of Eating Disorders, Children’s
Minnesota,
Minneapolis, MN, USA
Full list of author information is available at the end of the
article
Eckhardt et al. Journal of Eating Disorders (2019) 7:34
https://doi.org/10.1186/s40337-019-0267-x
http://crossmark.crossref.org/dialog/?doi=10.1186/s40337-019-
0267-x&domain=pdf
http://orcid.org/0000-0003-0824-4328
http://creativecommons.org/licenses/by/4.0/
http://creativecommons.org/publicdomain/zero/1.0/
mailto:[email protected]](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-269-320.jpg)
![UP for ARFID was developed through a 3 year case
consultation process with treatment developers of both
FBT and the UP-C. Treatment focuses on a combination
of techniques aimed at addressing both weight gain/
normalization of eating and additional symptoms includ-
ing fear, disgust, and worry or obsessive thoughts, as
well as varying forms of functionally-related avoidance
behavior and potential concomitant reinforcement of
avoidance by parents/caregivers. A major advantage of
this combined approach is that it allows the clinician to
personalize treatment based on the patient’s specific
presentation using a core set of evidence-based strategies
and assessment tools (e.g., Top Problems [16];). The
UP-C is transdiagnostic by definition, and contains
evidence-based strategies that are flexible enough to
address many of the maintaining symptoms that are
unique to ARFID. There is also an adolescent version of
the UP-C, which when combined with FBT makes this
treatment model acceptable for a wide range of patients
(named the Unified Protocol for Transdiagnostic Treat-
ment of Emotional Disorders in Adolescents; UP-A).
The UP for adults has previously been adapted for use
with other eating disorder populations (anorexia nervosa,
bulimia nervosa, and binge-eating disorder), with early
results indicating improvments in anxiety sensitivity, ex-
periential avoidance, and mindfulness [17].
While flexible, FBT + UP for ARFID always begins with
sessions focused on FBT principles, including collabora-
tive weighing, psychoeducation (specific to ARFID pa-
tients and their eating problems), family engagement,
separating the eating problem from the child, charging
parents with taking control of their child’s eating (includ-
ing increasing volume and variety of foods), promoting
weight gain as needed, and a family meal. The UP-C or](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-270-320.jpg)
![UP-A is then added to build skills that empower the
patient to cope with difficult emotions, address avoidance,
and increase tolerance of emotions or disgust responses.
The Unified Protocol for Transdiagnostic Treatment of
Emotional Disorders (UP) [18] is an emotion-focused,
evidence-based treatment that targets the core dysfunction
of neuroticism in adults [19]. It has subsequently been
adapted to address emotional disorders in youth with the
development of the Unified Protocols for Transdiagnostic
Treatment of Emotional Disorders in Children and Ado-
lescents (UP-C and UP-A respectively [15];). These proto-
cols bring together cognitive-behavioral techniques, such
as cognitive reappraisal, problem-solving and opposite
action strategies, including a variety of exposure para-
digms and behavioral activation, as well as mindfulness
techniques into a single treatment. The UP-C and UP-A
present the same skills as the UP; however, the skills have
been adapted to be developmentally sensitive in their
presentation, as well as in their delivery. Furthermore, the
UP-C and UP-A also target core emotional parenting
behaviors that are common across emotional disorders in
youth (i.e. high levels of criticism, over-control/over
protection, inconsistency, and modeling of avoidance
[15]). Research has provided support for the efficacy and
feasibility of the UP, UP-A and UP-C for individuals with
mood, anxiety, and other emotional disorders. The UP,
in particular, has been shown to lead to significant
improvements at post-treatment [20], as well as main-
tenance of gains at follow-up time points [21] . The
UP-C was originally designed as a group version of the
UP-A, with concurrent child and parent group content.
However, the UP-C may be delivered in an individual
therapy model and explicit directions for doing so are
presented in the therapist guide. Preliminary evidence
suggests the UP-C may be similarly effective to leading](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-271-320.jpg)
![CBT approaches for childhood anxiety, with potential
benefits for those youth with higher levels of parent-
reported sadness, dysregulation or depressive symptoms
[22, 23]. The UP-A has also been shown to improve
symptoms of emotional disorders in adolescents. Re-
sults from multiple baseline, open-trial and initial wait-
list controlled trial studies showed that adolescents
evidenced significant improvement in their symptoms
after receiving 16 sessions of treatment using the UP-A
and gains were maintained at follow-up time points
[24–26]. While results of initial patient outcomes for
this combined FBT + UP for ARFID approach are not
yet available (given this treatment is currently being
studied as part of a larger, clinic-wide effectiveness
study), feedback from individual patients and practi-
tioners who have been trained in the model through a
clinical teaching day at the Academy of Eating Disor-
ders International Conference has been positive [27].
Consent to share the following case was provided by
the family and patient. Changes in identifying informa-
tion were made to protect patient privacy.
Case presentation
“Laura” is a nine-year-old female, who presented with 38
lbs. of weight loss, poor oral intake, and medical instability
in the context of fears about eating/choking secondary to
a recent diagnosis of gluten intolerance. Ten months be-
fore she presented for treatment, Laura felt unwell after
eating at a restaurant with her family. Following this ex-
perience, she became more anxious with eating, reporting
frequent stomach aches and headaches. Laura’s family
tried a variety of elimination diets, including stopping all
dairy and gluten. Laura was seen multiple times by her
pediatrician, who ultimately recommended allergy and
celiac testing. Over the course of this time Laura lost 29%
of her overall body weight. Laura’s symptoms continued](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-272-320.jpg)

![ation anxiety. Given Laura had previously trended at or
above the 85th percentile for BMI, the goal was to return
her weight back to her personal healthy weight range.
The underlying assumption of FBT + UP for ARFID is
that patients diagnosed with ARFID need a combination
of treatment techniques that focus on both weight gain
and/or normalizing eating while also addressing add-
itional emotional disorder symptoms (i.e. anxiety, de-
pression, obsessive-compulsive symptoms, emotional/
situational avoidance). Patients and their parents begin
with traditional FBT for several sessions (see Table 1 for
content). Once progress with weight gain/regular eating
are underway, the UP-C or UP-A modules are intro-
duced. The UP-C has a flexible approach with core
evidence-based principles and concurrent parenting
content for emotional disorders that can be individual-
ized for specific ARFID presentations [15]. Once the
UP-C is added, the session breakdown continues as
follows: 5 min weigh-in and update from patient on how
eating is progressing, 30–40 min of individual therapy
with the patient focused on the UP-C content, and 10–
15 min with the patient and family to review session
content, discuss how eating/weight gain are progressing,
brainstorm challenges related to eating, and review
homework/exposure practice. For younger patients,
parents may be present for more/all of the session.
As illustrated in Table 2, over the course of treatment
Laura’s weight increased from 36.7 kg to 44.7 kg (percent
goal weight from 81.4 to 91.4%), with family noting
significant improvements in energy level and ability to
participate in school and other physical activities. During
initial FBT sessions, the focus was on weight gain using
foods that Laura felt were safe and could allow her to re-](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-274-320.jpg)
![gain weight efficiently. In session two, a family meal was
completed, where the therapist worked to separate the
illness from Laura and decrease blame (see FBT manual
[14]), as well as discuss rewards that could be utilized to
encourage Laura to challenge herself with eating. After
two sessions of FBT (and with Laura’s weight increas-
ing), the UP-C was added to sessions, though the focus
of each subsequent session also remained on weight
regain and parental support/empowerment. Of note,
Laura’s family took to the principles of FBT quickly, but
continued to benefit from each session’s focus on graph-
ing the patient’s weight, problem solving any challenges
during weeks where weight was stable or down, and
empowering parents to work closely together on how to
best refeed their daughter.
The patient and family identified three Top Problems
(an ideographic assessment tool by Weisz et al. [16]
modified for use in the UP-C and UP-A by Ehrenreich-
May et al. [15]) they wanted to address in treatment
including: 1) decrease fears of choking/eating feared
foods, 2) be away from/eat away from mother, and 3)
patient sleeping in her own bed again. Additionally, the
therapist reinforced an overarching goal of Laura return-
ing to a healthy weight range as crucial for her recovery.
All subsequent treatment sessions involved reviewing
Laura’s weight/eating, teaching content from the UP-C
modules, and discussing home learning assignments.
As treatment progressed and the patient learned skills
to better manage her emotions, she became more willing
to try foods that she was avoiding. With the help of the
treating clinician, Laura created an exposure hierarchy
with numerous feared foods and situations (e.g. meats,
pasta, nuts, eating with adults other than her mother,
eating at restaurants, being away from her mother, and](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-275-320.jpg)


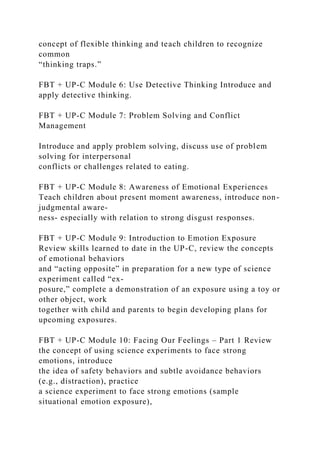

![and decrease anxiety about eating/being away from her
mother. Notably, when this family returned for a follow-
up 5 months after completing treatment, the patient’s
weight had continued to increase (50.4 kg/81st percentile
for BMI/97.1% of goal weight), she had started menstru-
ating, and she was able to separate and eat apart from
her mother without significant difficulty. The patient
and parents also rated her fears of choking and eating
previously feared foods as 1 and 2’s on an 8-point likert
scale (see Table 2).
This patient was a good treatment candidate for FBT +
UP for ARFID given she endorsed significant anxiety prior
to treatment and also met criteria for several concurrent
anxiety disorder diagnoses. Another major benefit of the
treatment is the ability to flexibly offer the various modules
that may benefit each patient based on their specific needs
and ARFID presentations. For example, this patient bene-
fited from exposure work, learning non-judgmental aware-
ness, and improving awareness of physical sensations,
while other patients may need more focus on cognitive
reappraisal, problem-solving, and other types of opposite
action [15]. Additionally, given Laura had lost a significant
amount of weight she required a treatment that also
focused on weight restoration as one of its core principles.
A major advantage of this combined treatment approach is
the ability for clinicians to tailor each session to the specific
needs of their individual patient, including returning to
solely FBT sessions if weight gain or nutritional dificiencies
are not progressing appropriately.
While several novel approaches for the treatment of
ARFID have been suggested [7, 10, 11], randomized con-
trol trials have yet to be presented regarding their effi-
cacy. Even with some intervention research aiming to](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-281-320.jpg)
![address the heterogeneous symptoms of ARFID, no
treatment to date has proposed a model that addresses
both the varied presentations of ARFID, as well as its full
range of common comorbid disorders, in one cohesive
approach that is flexible and adaptable to the individual.
While the development of symptom specific treatment
approaches to ARFID is logical, it does not address the
heterogeneous nature of this disorder and can impede
dissemination [28]. With so many different presentations
of ARFID and high rates of comorbid disorders, one
clear treatment that can be used flexibly to adapt to the
range of ARFID presentations and co-occurring disorders
would provide an efficient and cohesive approach to treat-
ing youth with ARFID. Further examination of FBT + UP
for a wide-range of ARFID presentations among youth
continues. A study to establish an ideal combination of
FBT and UP strategies for youth with ARFID between the
ages of 6–18 years, and the preliminary efficacy of this ap-
proach, is a next logical step in this research.
Finally, some limitations with this case study should
be noted. First, it was not possible to ascertain whether
FBT in isolation would have worked as effectively for
this patient as this combined FBT + UP-C approach.
While anxiety reduction has been shown in nutritional-
based therapies, such as FBT, it is unclear if patients
with profound phobic and other concurrent anxiety
would benefit as greatly without specific skills and expos-
ure work inherent in the UP-C. Additional limitations of
this case study include the absence of objective assessment
of psychological outcomes. That said, this young person
made significant improvements in terms of weight, both at
completion of treatment and at follow-up. Moreover, Top
Problems rating by both the patient and parents also
appear to indicate meaningful improvements in a variety of
behavioral domains. However, without objective measures](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-282-320.jpg)



![25. Ehrenreich JT, Goldstein CR, Wright LR, Barlow DH.
Development of a
unified protocol for the treatment of emotional disorders in
youth. Child
Family Behav Ther. 2009;31(1):20–37.
26. Queen AH, Barlow DH, Ehrenreich-May J. The trajectories
of adolescent
anxiety and depressive symptoms over the course of a
transdiagnostic
treatment. J Anxiety Disord. 2014;28(6):511–21.
27. Lesser JK, Eckhardt S, Le Grange D, Ehrenreich-May J.
Integrating family
based treatment with the unified protocol for the transdiagnostic
treatment
of emotional disorders: A novel treatment for avoidant
restrictive food
intake disorder. Prague: Academy of Eating Disorders
International
Conference; 2017. [Clinical teaching day]
28. McHugh RK, Barlow DH. The dissemination and
implementation of
evidence-based psychological treatments: a review of current
efforts. Am
Psychol. 2010;65(2):73.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional
claims in
published maps and institutional affiliations.
Eckhardt et al. Journal of Eating Disorders (2019) 7:34
Page 7 of 7](https://image.slidesharecdn.com/httpswww-221015083550-d2f85022/85/httpswww-nationaleatingdisorders-orglearnby-eating-disordera-docx-292-320.jpg)
