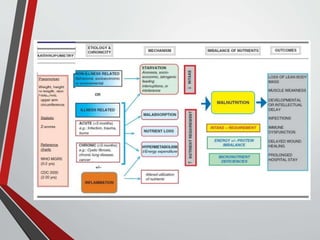
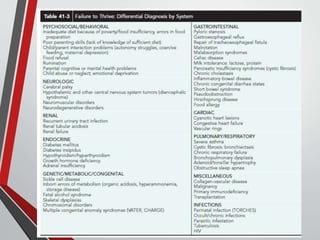
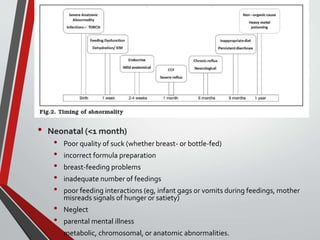
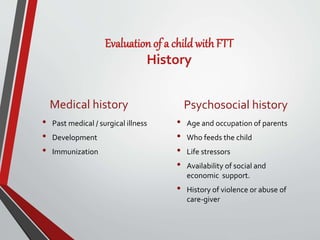
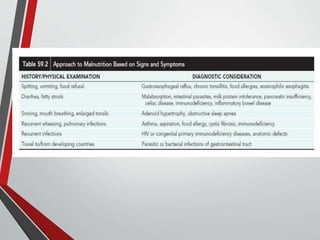
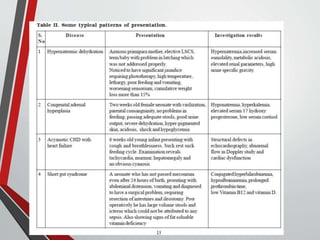
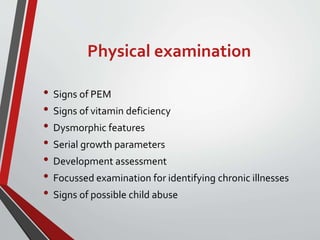
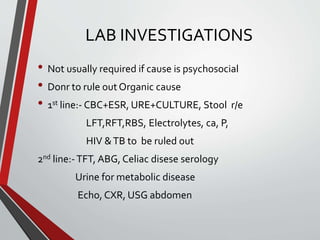
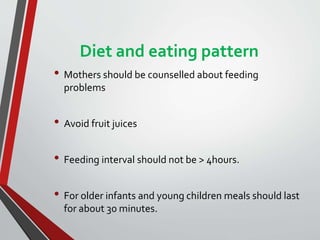
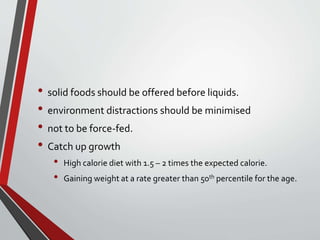
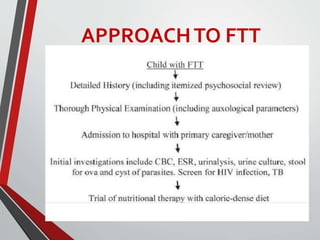
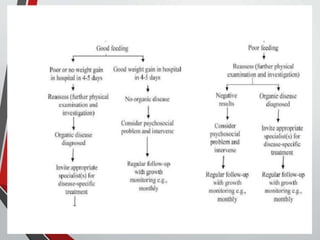
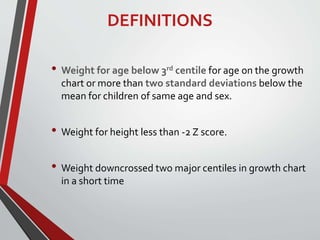
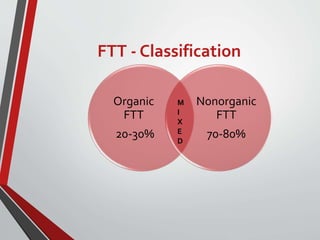
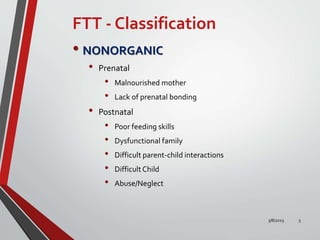
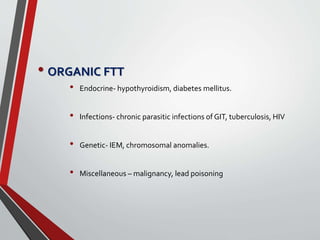
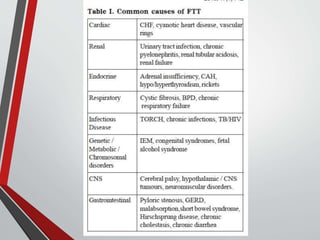
Failure to thrive (FTT) is a descriptive term used for infants and children under 3 years whose growth is significantly less than peers. It can be organic (20-30%) due to medical causes, or nonorganic (70-80%) due to environmental factors. Evaluation of a child with FTT involves obtaining a thorough history, physical exam, anthropometry, and investigations if needed to rule out organic causes. Management focuses on improving the child's diet and eating patterns, developmental stimulation, enhancing the caregiver's skills, treating any underlying diseases, and regular follow-up to monitor the effectiveness of nutritional therapy.



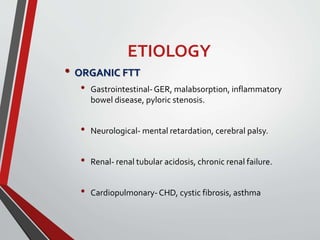
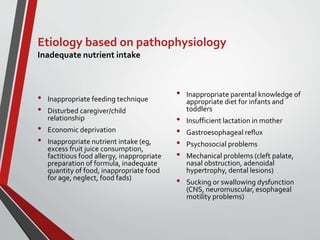
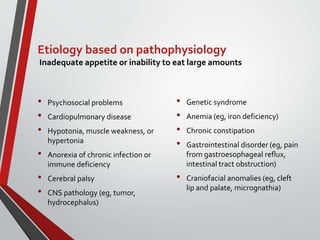
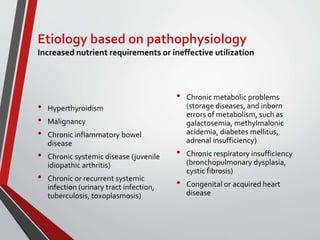
![Etiology based on pathophysiology
Inadequate nutrient absorption or increased losses
• Malabsorption
• Biliary atresia, cirrhosis
• Vomiting or "spitting up" (related
to infectious gastroenteritis,
increased intracranial pressure,
adrenal insufficiency, or drugs [eg,
purposeful administration of syrup
of ipecac])
• Intestinal tract obstruction (pyloric
stenosis, hernia, malrotation,
intussusception)
• Infectious diarrhea
• Necrotizing enterocolitis or short
bowel syndrome](https://image.slidesharecdn.com/failuretothrive-230308082301-1f512848/85/FAILURE-TO-THRIVE-pptx-14-320.jpg)