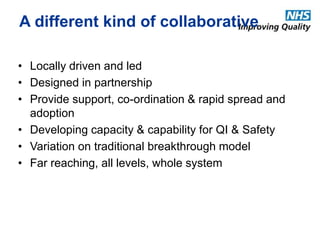
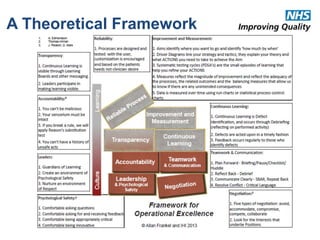
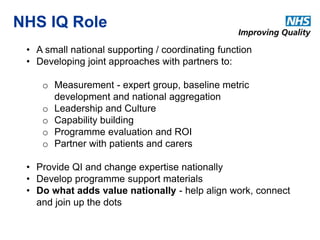
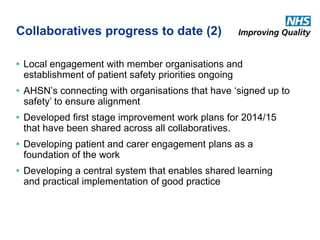
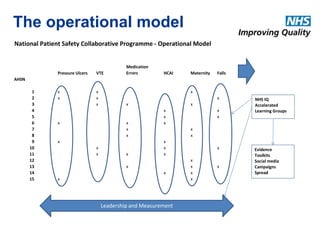
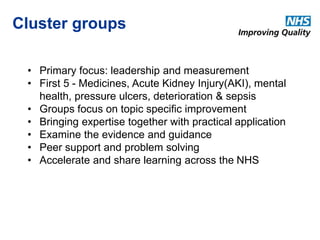
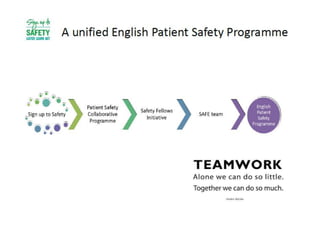
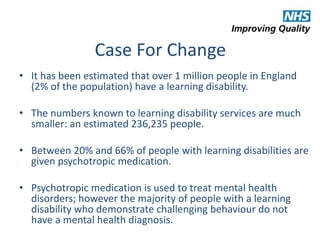
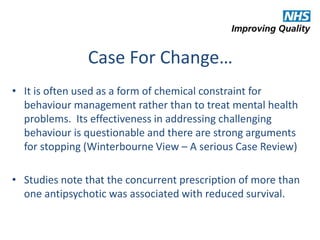
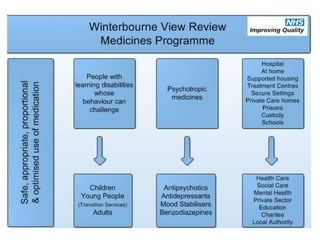
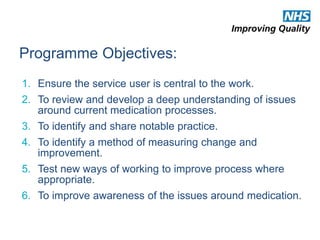
The document outlines the NHS's Patient Safety Collaborative Programme from 2014-2019, aimed at improving patient care and safety by fostering continuous learning and improvement across the healthcare system. It emphasizes the importance of active participation from NHS staff, patients, and caregivers in enhancing care quality and addresses the over-prescription of psychotropic medications for individuals with learning disabilities through the Winterbourne Medicines Programme. The document also details the collaborative's operational model, objectives, and partnerships established to ensure effective medication management and safety practices.