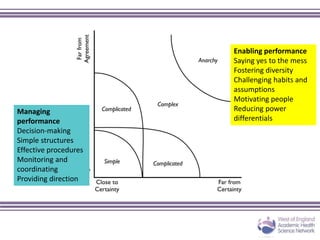
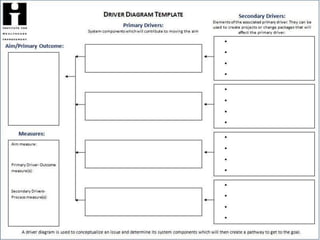
The document details the launch of the Primary Care Collaborative by the West of England Academic Health Science Network, focusing on improving patient safety in primary care through innovation and a culture of continual learning. It outlines strategies for developing a safety culture, including the use of PDSA cycles for quality improvement, and emphasizes collaborative efforts among healthcare professionals. Additionally, it presents a framework designed to assess and enhance patient safety practices within GP practices across the region.

































































































![Wessex Patient Safety Collaborative
Connecting and sharing across Wessex to improve patient safety
• The safe practice framework was developed by a number of GPs and
Primary Care Commissioners and agreed by Wessex Patient Safety
Collaborative [WPSC] Primary Care Forum.
• Test specification and measurement strategy was developed to measure
the impact of any change.
• The framework was tested by GP
practices.
• Framework was reviewed following feedback
and amended.
How?](https://image.slidesharecdn.com/primarycarecollaborative224-170525081900/85/Primary-Care-Collaborative-2-102-320.jpg)

![Wessex Patient Safety Collaborative
Connecting and sharing across Wessex to improve patient safety
• Feedback itself is crucial to ensure the framework is useful for you.
• The feedback we received;
• Most useful when completed as a team.
• Each team member had ownership of the good
practice that was identified and wanted to take
responsibility for what needed to change.
• Local Medical Council [LMC] Chief Executive
saw value in the framework.
• Rewritten to reflect Key Lines of Enquiry and as a 2 stage approach.
• Not an assurance tool.
Feedback!](https://image.slidesharecdn.com/primarycarecollaborative224-170525081900/85/Primary-Care-Collaborative-2-104-320.jpg)







