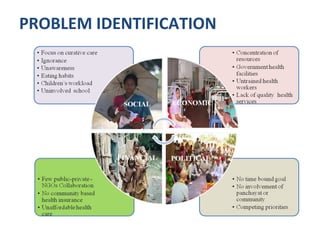
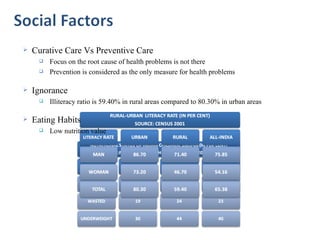
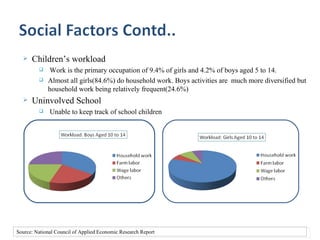
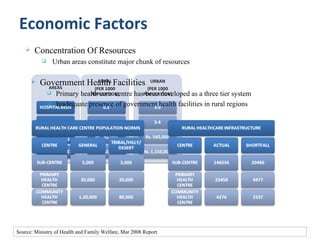
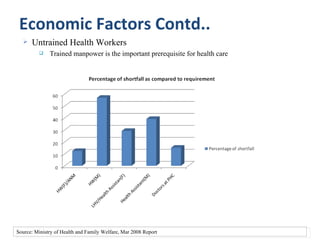
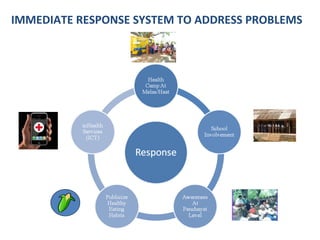
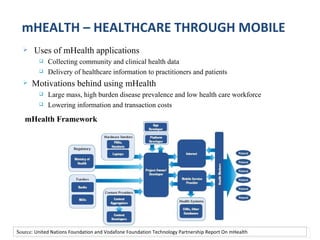
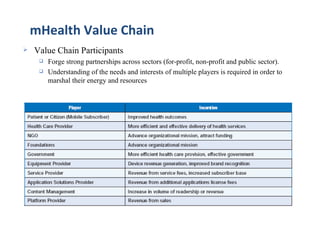
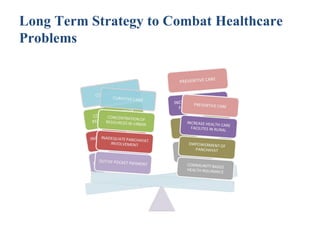
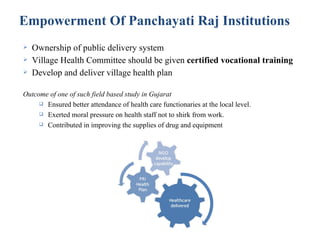
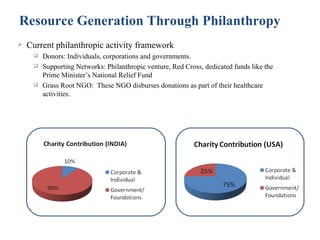
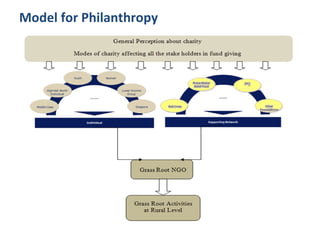
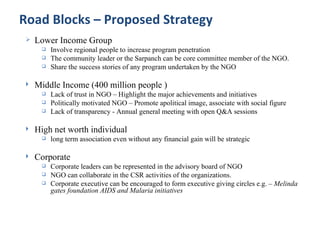
This document presents a case study on developing a long-term strategy to combat health care problems among underprivileged people in India. It identifies key problems such as a focus on curative rather than preventive care, illiteracy, poor nutrition, children's workloads, and a lack of involvement from schools. Immediate responses proposed include using mobile health applications, organizing health camps, and encouraging collaborative efforts between different actors. The long-term strategy focuses on preventive health services, improving infrastructure and services through increased resources and public-private partnerships, empowering local governments, implementing community-based health insurance, and generating resources through targeted philanthropy programs. Roadblocks to implementation are also addressed.