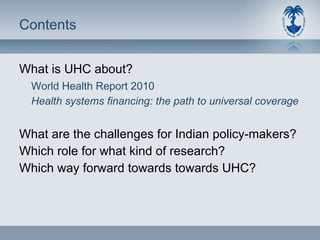
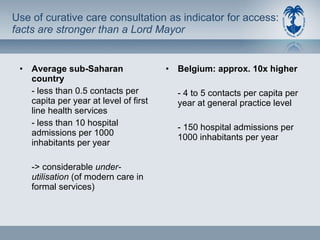
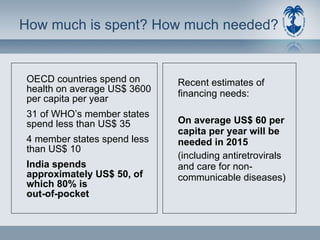
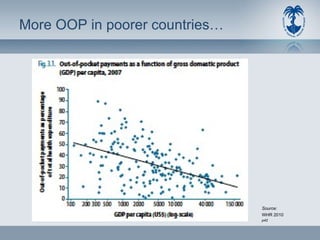
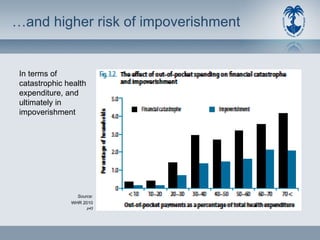
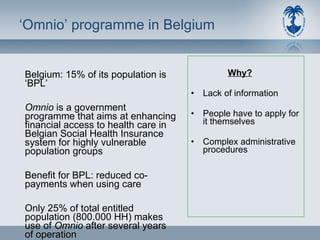
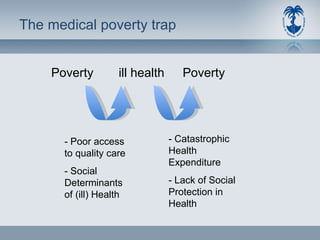
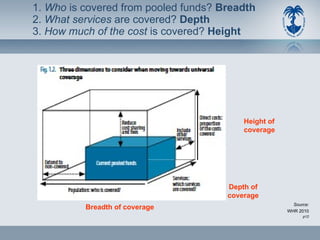
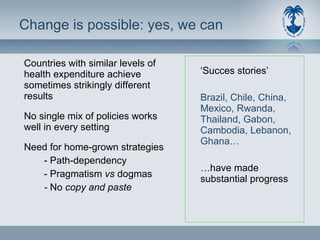
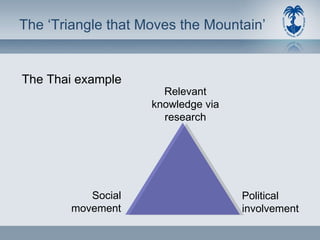
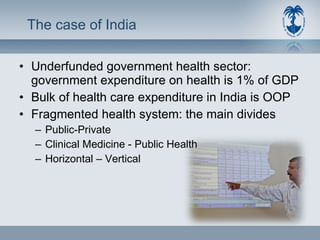
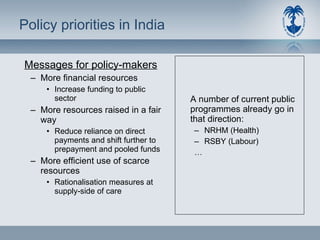
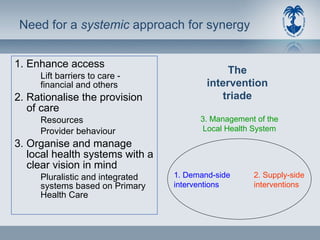
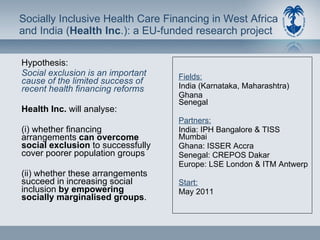
This document discusses universal health coverage (UHC) and challenges in achieving it. It notes that UHC aims for all people to access health services without financial hardship. Achieving UHC requires more resources, raising funds fairly, and efficient spending. Most countries spend too little. Out-of-pocket payments deter use and impoverish people. Pooled funds through prepayment are better. Research is needed to understand inequities and improve programs. Community involvement may help transform health insurance for the poor. More comprehensive systems combining financial, supply, and management reforms are needed to organize accessible, quality care for all.