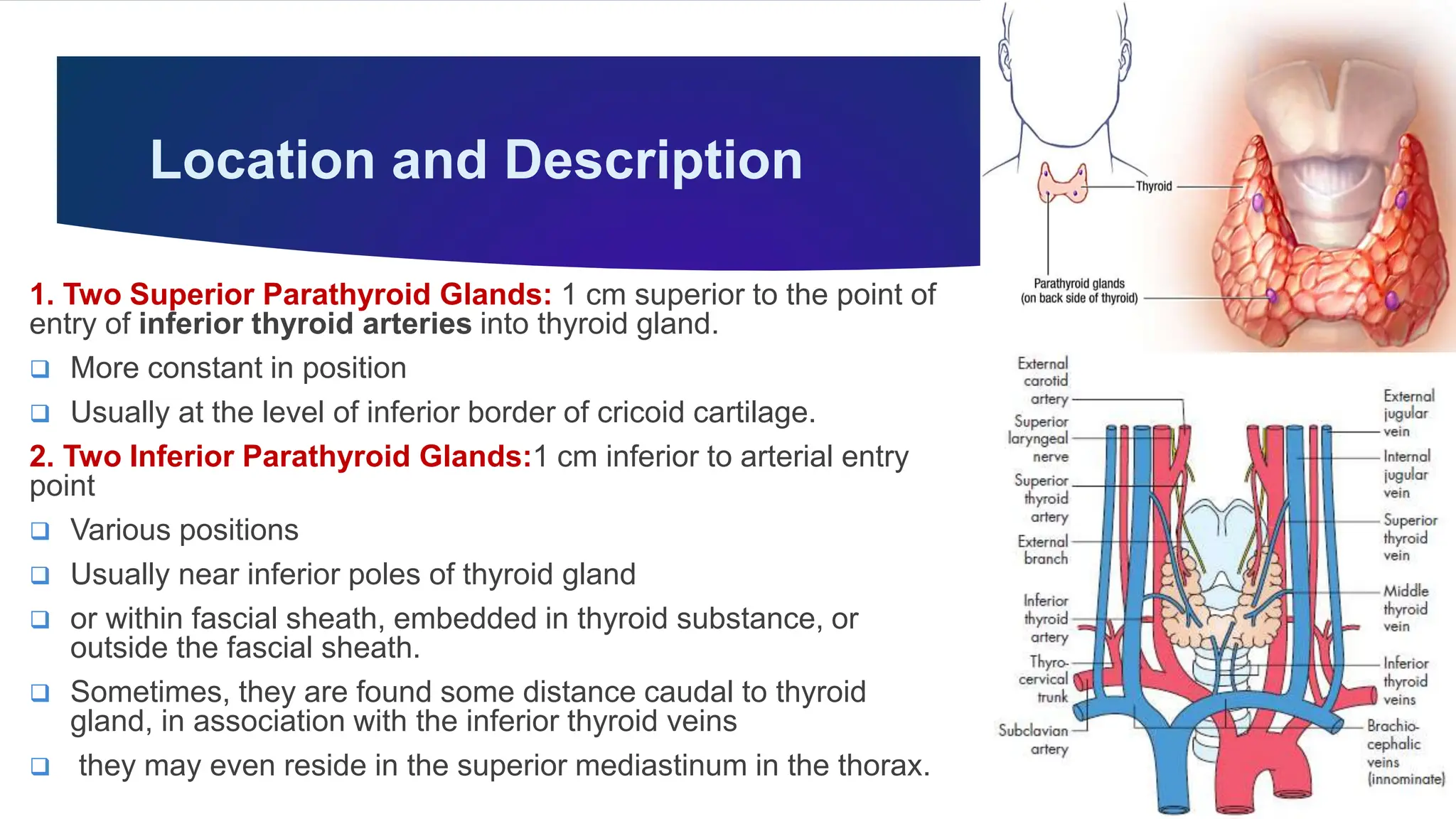
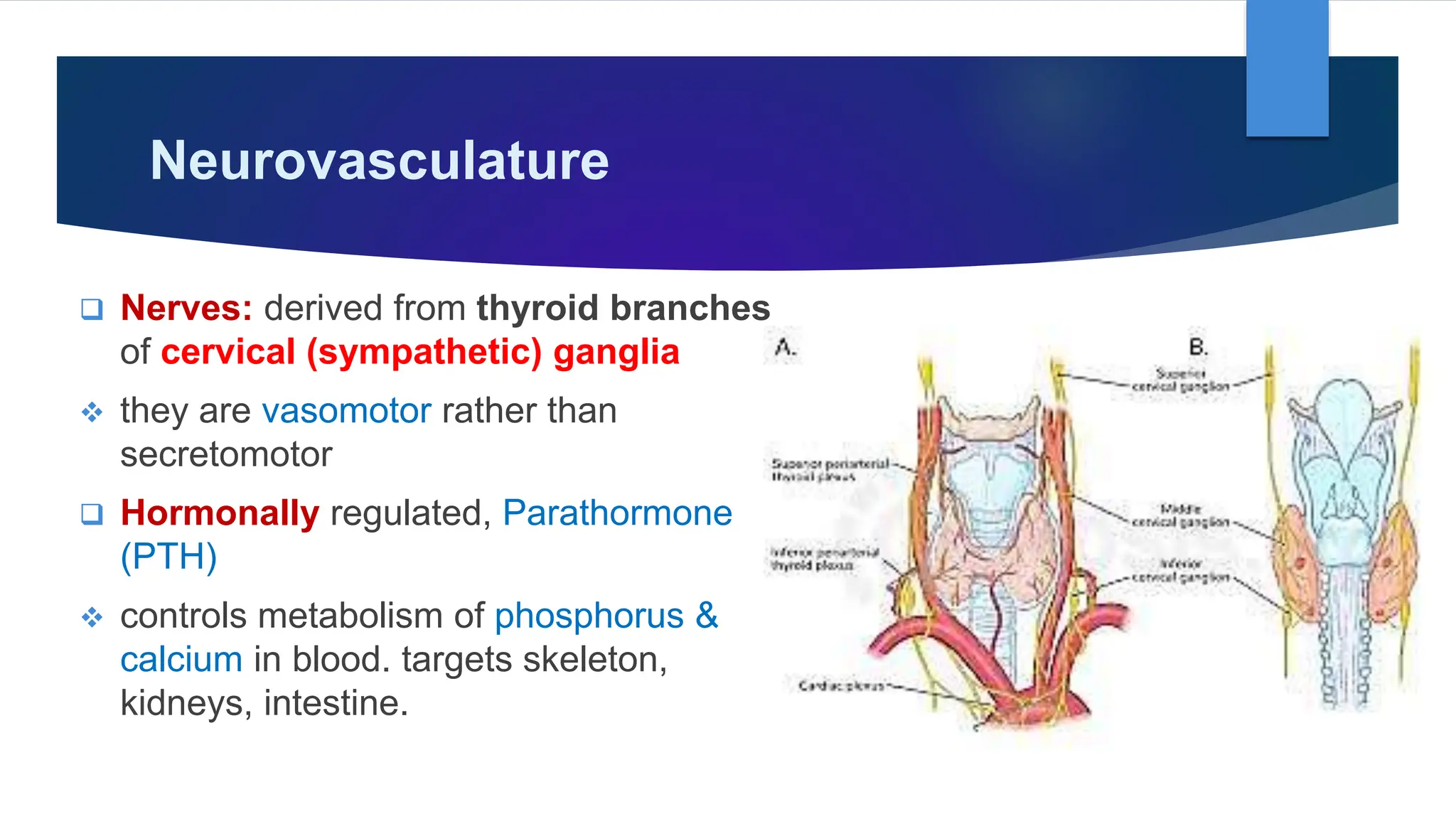
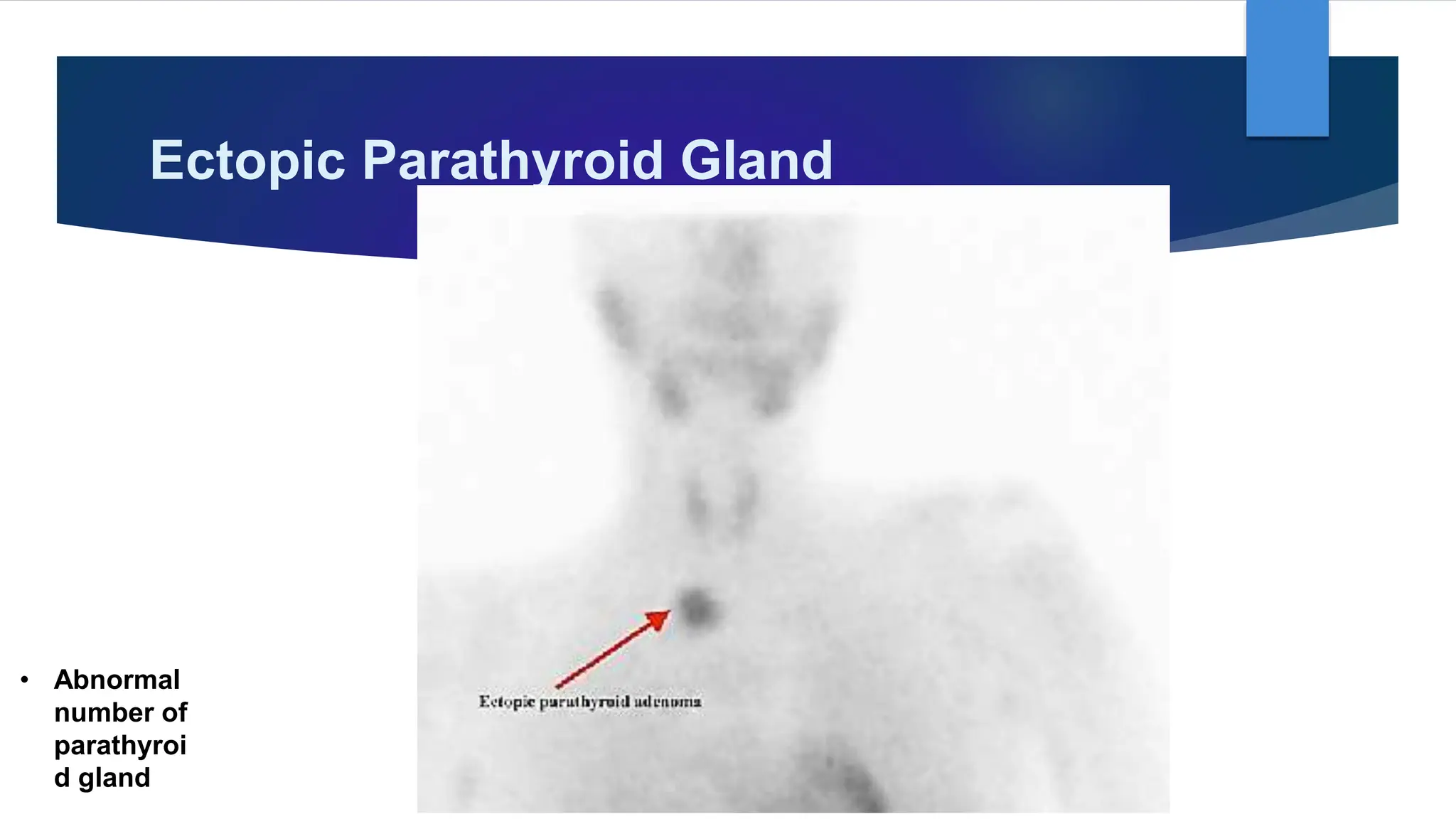
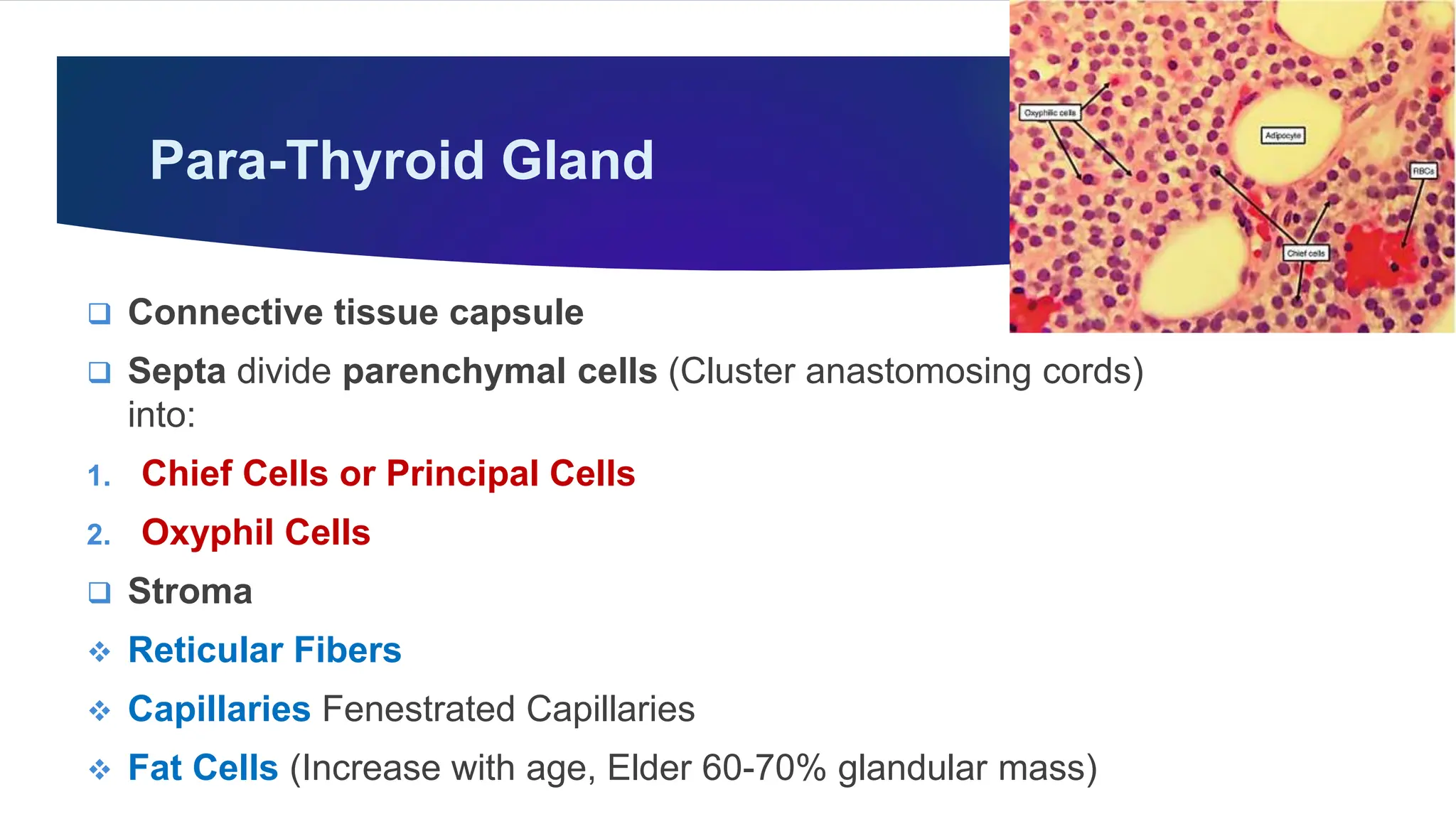
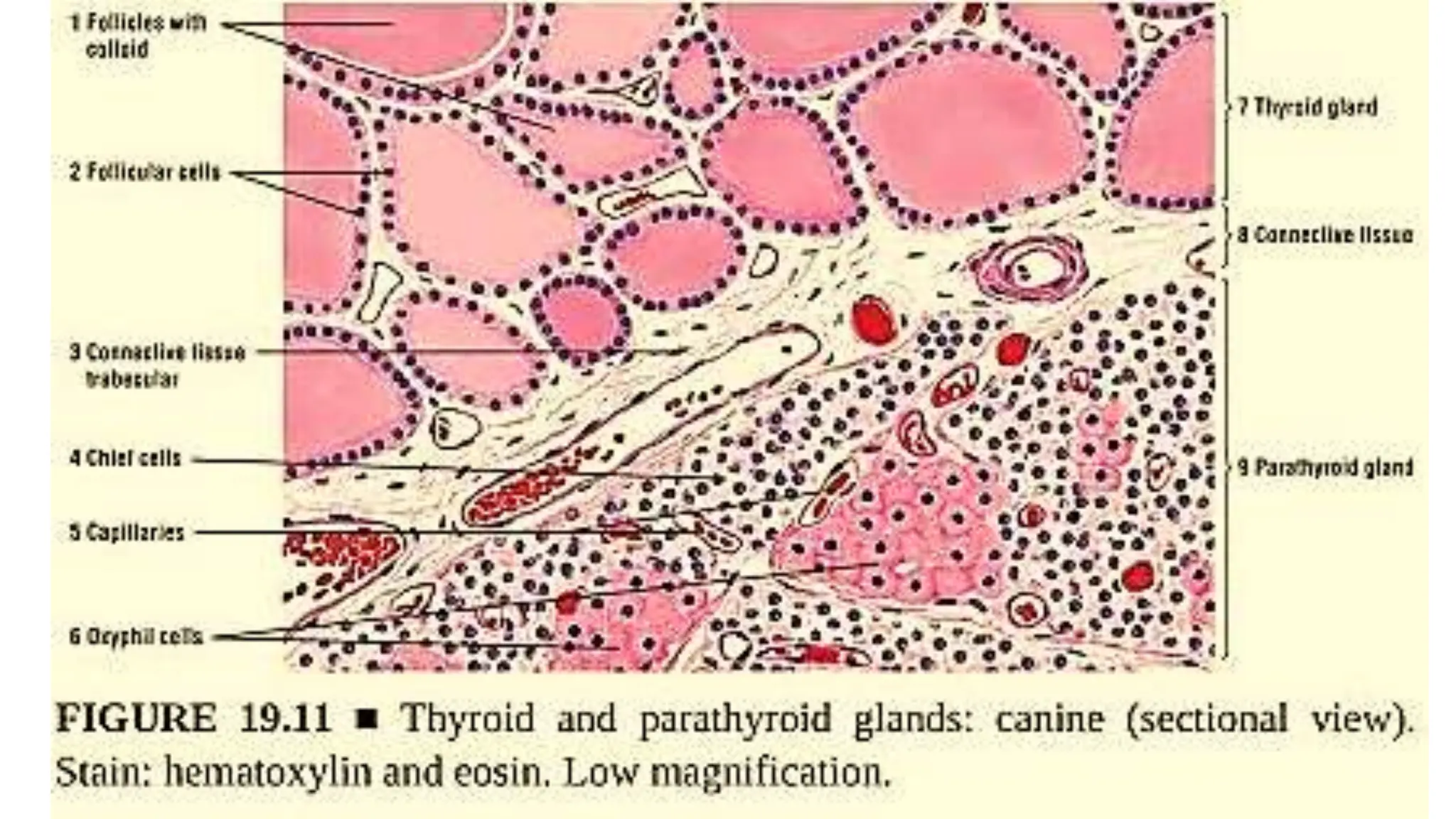
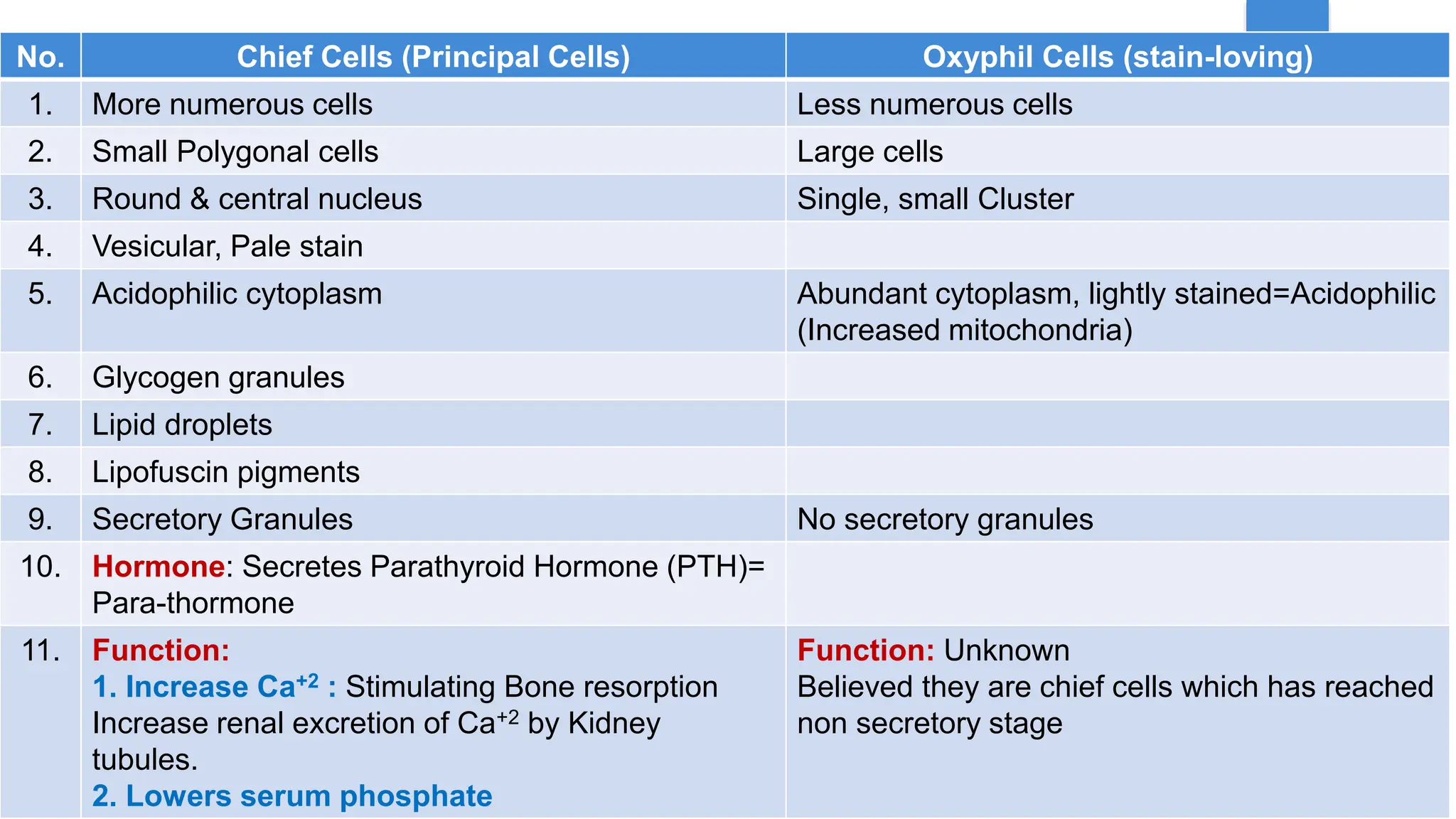
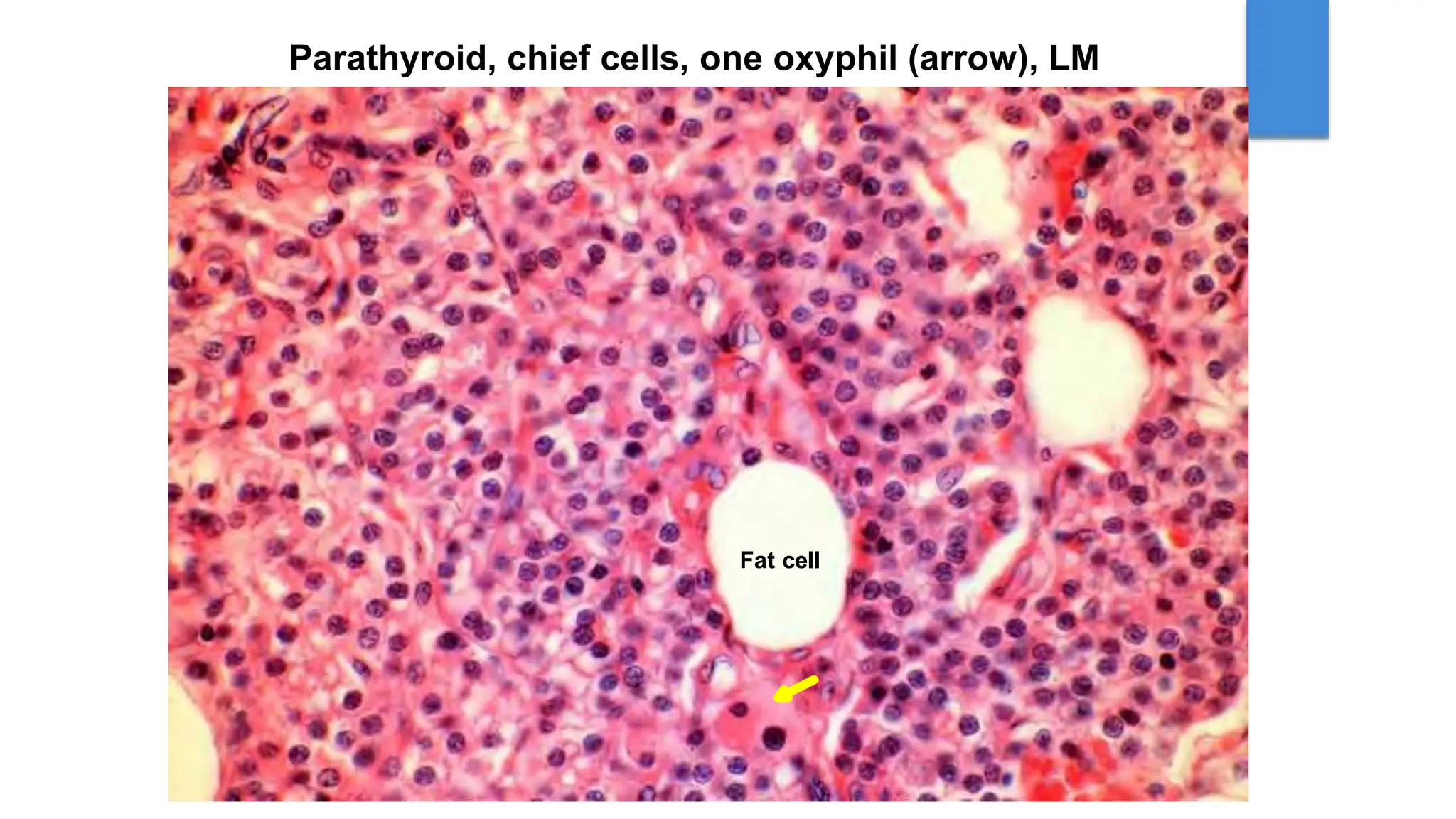
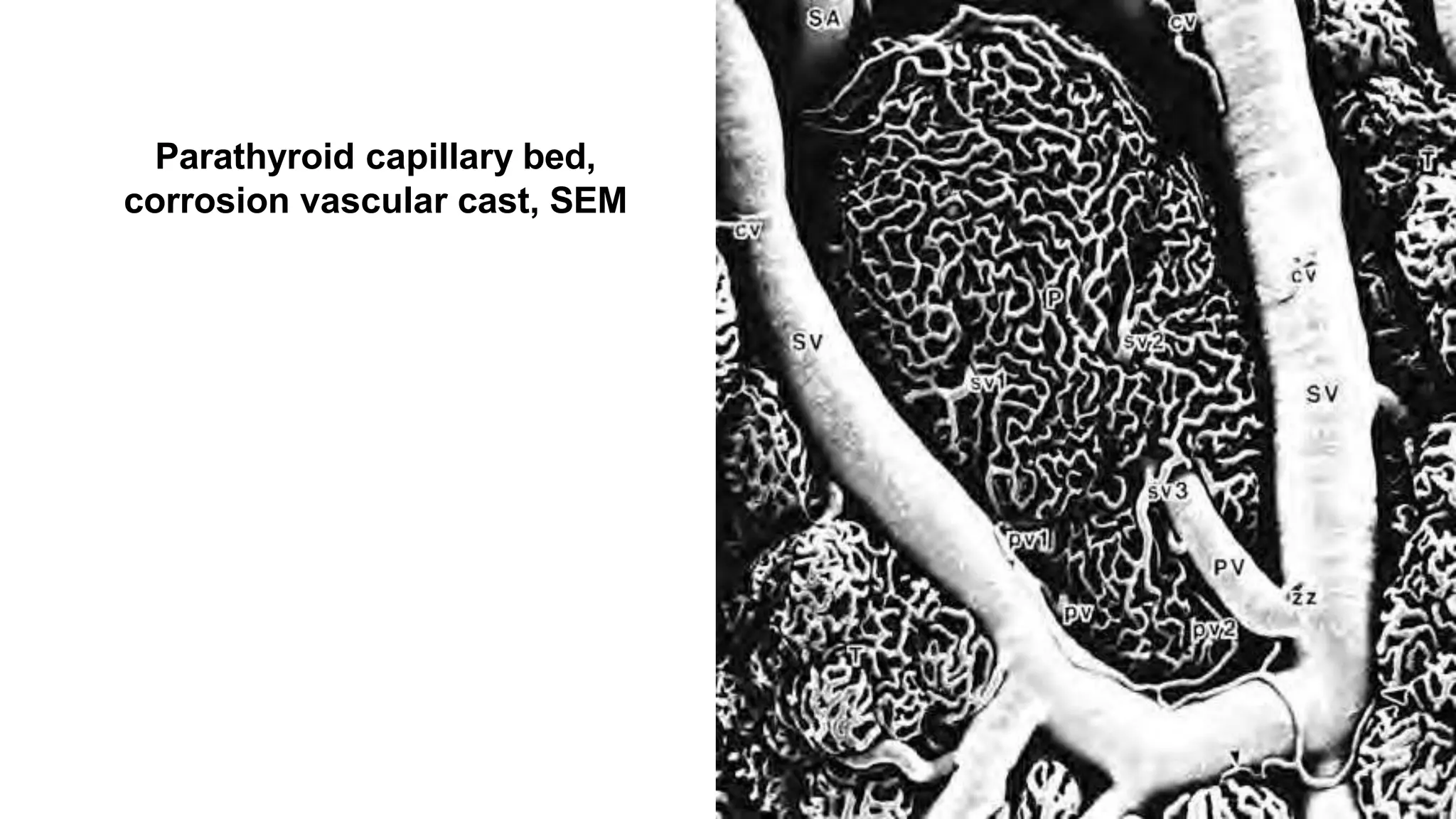
The document outlines the gross anatomy and histology of the parathyroid glands, detailing their location, structure, function, and blood supply. It describes the teaching methodologies employed to facilitate student learning, including various interactive and self-directed learning approaches. Additionally, it covers the histological features, clinical correlations, and the role of parathyroid hormone in regulating calcium and phosphate levels in the body.