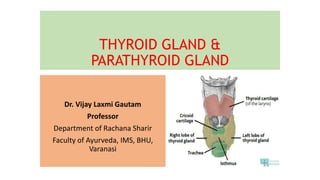
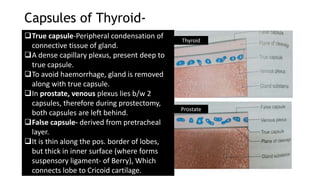
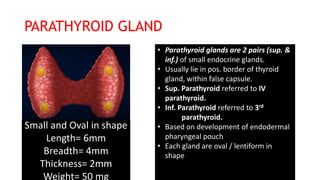
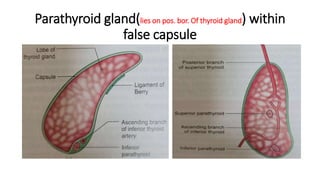
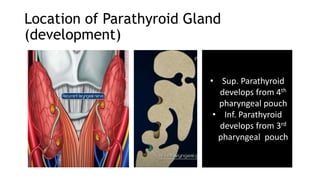
The thyroid and parathyroid glands are located in the neck. The thyroid gland regulates metabolism and consists of two lobes connected by an isthmus. It is supplied by the superior and inferior thyroid arteries. The parathyroid glands secrete parathyroid hormone which regulates calcium levels in the blood and are usually located on the back of the thyroid gland. Dysfunction of these glands can cause disorders like hypothyroidism, hyperthyroidism, hyperparathyroidism and hypoparathyroidism. During surgery on the thyroid gland, care must be taken to preserve the parathyroid glands and their blood supply.