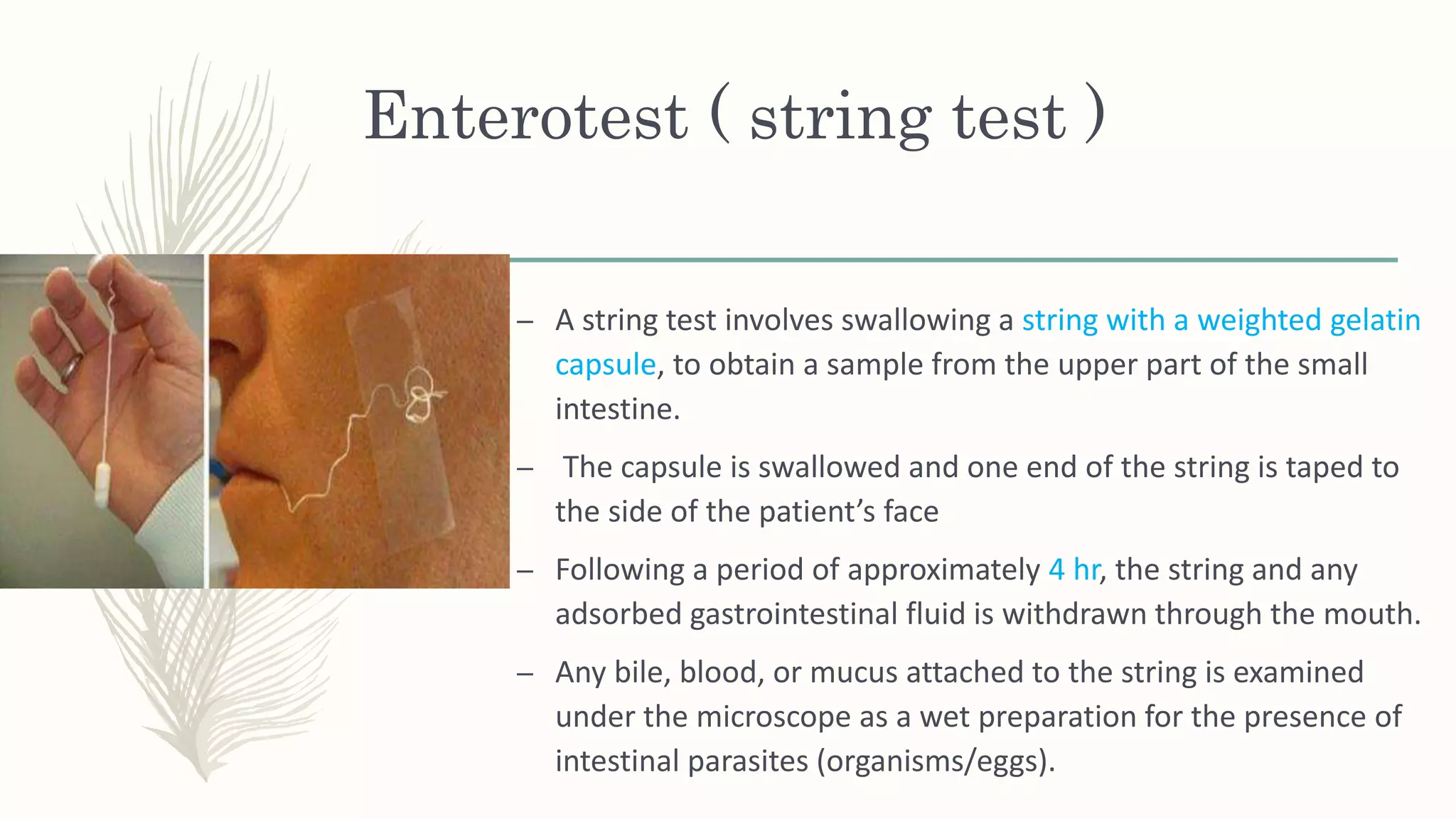
The document presents a case study of a child diagnosed with giardiasis, characterized by symptoms like nausea, anorexia, and diarrhea, accompanied by stool examination results. It elaborates on the morphology, life cycle, pathogenesis, clinical features, and laboratory diagnosis of Giardia lamblia, noting various treatment options and preventive measures. The document emphasizes that proper hygiene and water sanitation are crucial in managing and preventing infections.