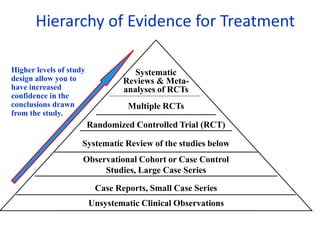
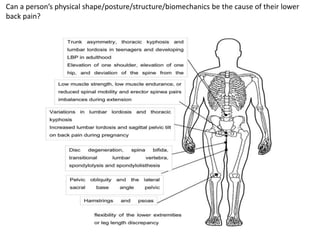
This document discusses a paradigm shift in spinal manual therapy from a biomechanical model to a neurophysiological model. It provides evidence that lower back pain is not caused by biomechanical factors like posture or spinal structure. While biomechanics was previously emphasized, evidence now shows biomechanics do not determine pain or pathology. The document advocates abandoning the postural-structural-biomechanical model and assessment of biomechanical factors in favor of a process-based approach focused on underlying neuromuscular processes rather than structure. Manual therapy should aim to facilitate changes in these processes rather than correct biomechanics, which are normal variations and cannot reliably be changed.