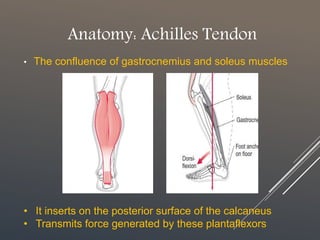
The document discusses achilles tendinopathy, a condition characterized by pain, swelling, and weakness of the achilles tendon due to micro-injuries. It explains the anatomy and biomechanics of the achilles tendon, emphasizing that the condition results from the tendon’s inability to adapt to strain, leading to degeneration. Various biomechanical causes and factors contributing to tendon overload are also outlined.