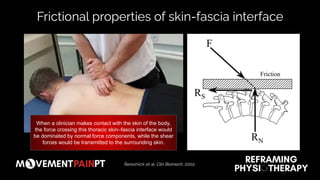
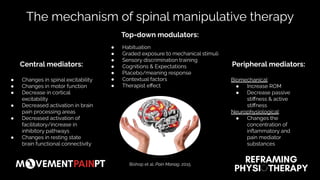
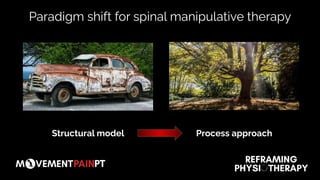
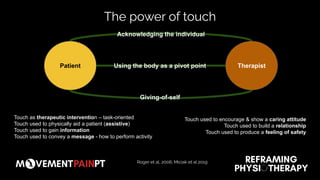
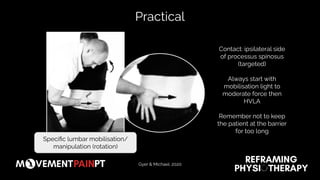
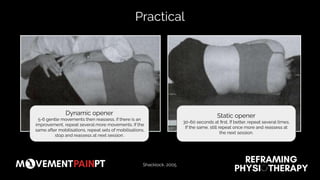
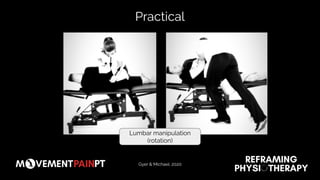
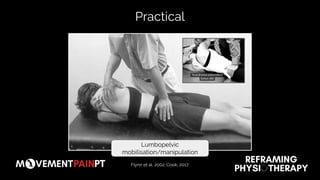
1. Spinal manipulative therapy is a process-based approach rather than one focused on structural fixes. It involves multiple potential mechanisms including changes in spinal excitability, motor function, and brain activation as well as peripheral factors.
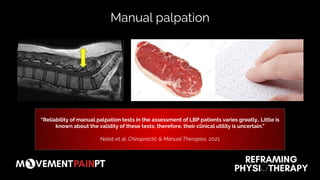
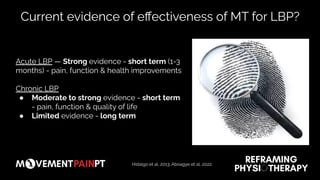
2. While manual palpation tests have uncertain validity and clinical utility, spinal manipulative therapy may provide short-term benefits for acute low back pain through mechanisms like increased range of motion and decreased stiffness.
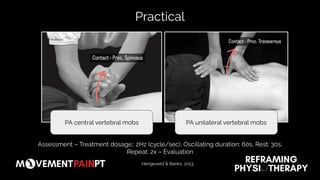
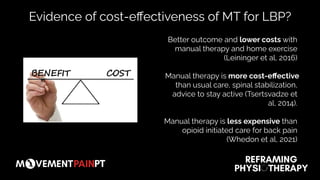
3. For optimal outcomes, spinal manipulative therapy should be combined with a home exercise program and delivered over multiple sessions rather than being viewed as an isolated treatment.