This document provides guidance on evaluating palpitations in children. It describes how to take a history regarding the sensations, triggers, and associated symptoms. A physical exam and ECG can help identify potential cardiac causes like arrhythmias. While most palpitations have non-serious causes like anxiety, further workup may be needed if risk factors are present like a family history of sudden cardiac death. Conditions like supraventricular tachycardia and long QT syndrome can potentially cause palpitations.











![Sinus tachycardia
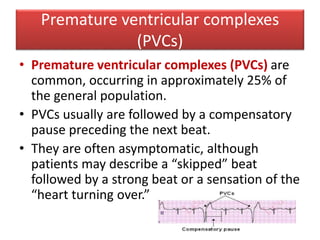
• Sinus tachycardia needs to be distinguished from supraventricular
tachycardia (SVT).
• Both are narrow complex tachycardias.
• Sinus tachycardia is characterized by a normal P-wave axis, a
gradual onset and termination, and a rate higher than the age-
specific upper limit of normal (usually less than 230 to 240 beats
per minute [bpm]); variability in the heart rate is a characteristic
distinguishing it from SVT.
• Fever, pain, anemia, and dehydration are common causes of sinus
tachycardia.](https://image.slidesharecdn.com/palpitationinchildren-180503080420/85/Palpitation-in-children-12-320.jpg)