MANAGEMENT OF PATIENTS WITH ARRHYTHMIAS milka.pptx
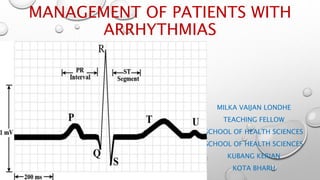
- 1. MANAGEMENT OF PATIENTS WITH ARRHYTHMIAS MILKA VAIJAN LONDHE TEACHING FELLOW SCHOOL OF HEALTH SCIENCES SCHOOL OF HEALTH SCIENCES KUBANG KERIAN KOTA BHARU
- 2. OBJECTIVES Define arrhythmias Explain the pathophysiology of arrhythmias Identify the manifestation of arrhythmias Apply the care plan of patients with arrhythmias
- 6. • RHYTHM DISTURBANCES RESULT FROM ABNORMALITIES OF IMPULSE FORMATION, IMPULSE CONDUCTION, OR BOTH. BRADY ARRHYTHMIAS RESULT FROM DECREASED INTRINSIC PACEMAKER FUNCTION OR BLOCKS IN CONDUCTION, PRINCIPALLY WITHIN THE AV NODE OR THE HIS-PURKINJE SYSTEM.
- 7. TYPES • SUPREVENTRICULAR ARRHYTHMIAS: • Atrial fibrillation • Atrial flutter • Atrial tachycardia • Atrioventricular nodal reentrant tachycardia • Paroxysmal supraventricular tachycardia • Wolff-Parkinson-white-syndrome
- 8. VENTRICULAR ARRHYTHMIAS: • Ventricular fibrillation • Ventricular tachycardia • Premature ventricular beats • Torsades de pointes INHERITED ARRHYTHMIAS: • Brugada syndrome • Catecholaminergic polymorphic ventricular tachycardia • Long QT syndrome BRADYCARDIA • Heart block • Sick Sinus Syndrome
- 9. ATRIAL FIBRILLATION • ATRIAL FIBRILLATION: • Is known as AF or afib, is an irregular, rapid heart rate that may cause symptoms like heart palpitations, fatigue, and shortness of breath. AF occurs when the upper chambers of the heart (atria) beat out of rhythm.
- 10. ATRIAL FLUTTER • It is a common abnormal heart rhythm that starts in the atrial chambers of the heart. When it first occurs, it is usually associated with a fast heart rate and is classified as a type of supraventricular tachycardia. • Although people with atrial flutter may not experience symptoms, the disorder can cause stroke, heart failure and other complications.
- 11. ATRIAL TACHYCARDIA • It is a type of abnormal heart rhythm, or arrhythmia. It occurs when the electrical signal that controls the heartbeat starts from an unusual location in the upper chambers (atria) and rapidly repeats, causing the atria to beat too quickly.
- 12. ATRIOVENTRICULAR NODAL REENTRANT TACHYCARDIA AV NODAL REENTRANT TACHYCARDIA (AVNRT), OR ATRIOVENTRICULAR NODAL REENTRANT TACHYCARDIA: • IS A TYPE OF ABNORMAL FAST HEART RHYTHM. IT IS A TYPE OF SUPRAVENTRICULAR TACHYCARDIA (SVT), MEANING THAT IT ORIGINATES FROM A LOCATION WITHIN THE HEART ABOVE THE BUNDLE OF HIS.
- 13. PAROXYSMAL SUPRAVENTRICULAR TACHYCARDIA PAROXYSMAL SUPRAVENTRICULAR TACHYCARDIA (PAROXYSMAL SVT) • Is an episodic condition with an abrupt onset and termination. SVT in general is any tachyarrhythmia that requires atrial and/or atrioventricular (AV) nodal tissue for its initiation and maintenance
- 15. WOLF-PARKINSON-WHITE SYNDROME CONTD…. • Wolff-Parkinson -white (WPW) syndrome is a condition in which there is an extra electrical pathway in the heart. The condition can lead to periods of rapid heart rate (tachycardia). • Wpw syndrome is one of the most common causes of fast heart rate problems in infants and children.
- 16. VENTRICULAR ARRHYTHMIAS • VENTRICULAR FIBRILLATION: Ventricular fibrillation is a heart rhythm problem that occurs when the heart beats with rapid, erratic electrical impulses. This causes pumping chambers in the heart (the ventricles) to quiver uselessly, instead of pumping blood. Sometimes triggered by a heart attack, ventricular fibrillation causes blood pressure to plummet, cutting off blood supply to the vital organs.
- 17. VENTRICULAR TACHYCARDIA VENTRICULAR TACHYCARDIA: • Is a very fast heart rhythm that begins in the ventricles. ... Ventricular tachycardia is a pulse of more than 100 beats per minute with at least three irregular heartbeats in a row. It is caused by a malfunction in the heart's electrical system.
- 18. PREMATURE VENTRICULAR BEATS PREMATURE VENTRICULAR CONTRACTIONS (PVCS) • ARE EXTRA HEARTBEATS THAT BEGIN IN ONE OF HEART'S TWO LOWER PUMPING CHAMBERS (VENTRICLES). THESE EXTRA BEATS DISRUPT REGULAR HEART RHYTHM, SOMETIMES CAUSING TO FEEL A FLUTTERING OR A SKIPPED BEAT IN THE CHEST.
- 19. INHERITED ARRHYTHMIAS • BRUGADA SYNDROME: IS A CONDITION THAT CAUSES A DISRUPTION OF THE HEART'S NORMAL RHYTHM. SPECIFICALLY • THIS DISORDER CAN LEAD TO IRREGULAR HEARTBEATS IN THE HEART'S LOWER CHAMBERS (VENTRICLES), WHICH IS AN ABNORMALITY CALLED VENTRICULAR ARRHYTHMIA.
- 20. CATECHOLAMINERGIC POLYMORPHIC VENTRICULAR TACHYCARDIA CATECHOLAMINERGIC POLYMORPHIC VENTRICULAR TACHYCARDIA (CPVT) • IS A GENETIC DISORDER THAT CAUSES AN ABNORMALLY FAST AND IRREGULAR HEART RHYTHM IN RESPONSE TO PHYSICAL ACTIVITY OR EMOTIONAL STRESS. ... WHEN A RYR2 GENE MUTATION IS INVOLVED, THE CONDITION IS PASSED THROUGH FAMILIES IN AN AUTOSOMAL DOMINANT FASHION.
- 21. LONG QT SYNDROME LONG QT SYNDROME (LQTS) IS • A heart rhythm condition that can potentially cause fast, chaotic heartbeats. • These rapid heartbeats might trigger a sudden fainting spell or seizure. ... And can have a genetic mutation that puts the person at risk of being born with congenital long qt syndrome
- 22. BRADYCARDIA HEART BLOCK is an abnormal heart rhythm where the heart beats too slowly (bradycardia ). • in this condition, the electrical signals that tell the heart to contract are partially or totally blocked between the upper chambers (atria) and the lower chambers (ventricles).
- 23. SICK SINUS SYNDROME SICK SINUS SYNDROME ( SSS ) • Is a relatively uncommon heart rhythm disorder. SSS is not a specific disease, but rather a group of signs or symptoms that indicate the sinus node, the heart's natural pacemaker, is not functioning properly.
- 24. RISK FACTORS • Coronary artery disease, other heart problems and previous heart surgery. • High blood pressure. • Congenital heart disease • Thyroid problems • . Drugs and supplements. Certain over-the-counter cough and cold medicines • Diabetes. • Obstructive sleep apnea • Electrolyte imbalance • Drinking too much alcohol. • Caffeine or nicotine use
- 25. CAUSES • Many things can lead to, or cause, an arrhythmia, including: • A heart attack that's occurring right now • Scarring of heart tissue from a prior heart attack • Changes to heart's structure, such as from cardiomyopathy • Blocked arteries in the heart (coronary artery disease) • High blood pressure • Overactive thyroid gland (hyperthyroidism)
- 26. CONTD….. • Underactive thyroid gland (hypothyroidism) • Smoking • Drinking too much alcohol or caffeine • Drug abuse • Stress • Certain medications and supplements, including over-the-counter cold and allergy drugs and nutritional supplements • Diabetes • Sleep apnea • Genetics
- 27. CLINICAL MANIFESTATION • A fluttering in the chest • A racing heartbeat (tachycardia) • A slow heartbeat (bradycardia) • Chest pain • Shortness of breath • Dizziness • Sweating • Fainting (syncope) or near fainting
- 28. PREVENTION • Eating a heart-healthy diet • Increasing physical activity • Avoiding smoking • Keeping a healthy weight • Limiting or avoiding caffeine and alcohol • Reducing stress, as intense stress and anger can cause heart rhythm problems • Using over-the-counter medications with caution, as some cold and cough medications contain stimulants that may trigger a rapid heartbeat
- 29. DIAGNOSTIC TESTS FOR ARRHYTHMIAS • Electrocardiogram • Holter monitor • Echocardiogram • Stress test
- 30. TREATMENT FOR ARRHYTHMIAS • ANTI-ARRHYTHMIC DRUGS • DEFIBRILLATION • PACEMAKER
- 31. ANTIARRHYTHMIC DRUGS CLASS I a AGENTS INTERFERE WITH THE SODIUM (NA+) CHANNEL. QUINIDINE AJMALINE PROCAINAMIDE DISOPYRAMIDE MECHANISM CLASS 1 PROLONG THE ACTION POTENTIAL AND HAS INTERMEDIATE EFFECT ON THE 0 PHASE OF DEPOLARIZATION MEDICAL USES VENTRICULAR ARRHYTHMIAS PREVENTION OF PAROXYSMAL RECURRENT ATRIAL FIBRILLATION (TRIGGERED BY VAGAL OVERACTIVITY) PROCAINAMIDE IN WOLFF-PARKINSON- WHITE SYNDROME INCREASES QT INTERVAL
- 32. CLASS 1b AGENT Na+ channel block (fast association/dissoci ation) Lidnocaine Phenytoin Nexiletine Tocainide MECHANISM Can prolong QRS complex in overdose Class 1b shorten the action potential of myocardial cell and has weak effect on intiation of phase 0 of depolarization MEDICAL USES Treatment and prevention during and immediately after myocardial infarction, though this practice is now discouraged given the increased risk of asystole Ventricular
- 33. CLASS 1 C AGENT NA+ CHANNEL BLOCK (SLOW ASSOCIATION/DISSO CIATION) ENCAINIDE FLECAINIDE PROPAFENONE MORICIZINE MECHANISM HAS NO EFFECT ON ACTION POTENTIAL AND HAS THE STRONGEST EFFECT ON INITIATION PHASE 0 THE DEPOLARIZATION MEDICAL USES PREVENTS PAROXYSMAL ATRIAL FIBRILLATION TREATS RECURRENT TACHYARRHYTHMIAS OF ABNORMAL CONDUCTION SYSTEM CONTRAINDICATED IMMEDIATELY AFTER MYOCARDIAL INFARCTION
- 34. CLASS 2 BETABLOCKERS Carvedilol Propranlol Esmolol Metaprolol Atenolol Bisoprolol Nebivolol MECHANISM BETA BLOCKING PROPRANOLOL ALSO SHOWS SOME CLASS I ACTION MEDICAL USES DECREASE MYOCARDIAL INFARCTION MORTALITY PREVENT RECURRENCE OF TACHYARRHYTHMIAS PROPRANOLOL HAS SODIUM CHANNEL- BLOCKING EFFECT
- 35. CLASS 3 K+ CHANNEL BLOCKER AMIODARONE SOTALOL IBUTILIDE DOFETILIDE DRONEDARONE E-4031 VERNAKALANT MECHANISM SOTALOL IS ALSO A BETA BLOCKER[4] AMIODARONE HAS CLASS III MOSTLY, BUT ALSO I, II, & IV ACTIVITY MEDICAL USES IN WOLFF-PARKINSON-WHITE SYNDROME (SOTALOL:) VENTRICULAR TACHYCARDIAS AND ATRIAL FIBRILLATION (IBUTILIDE:) ATRIAL FLUTTER AND ATRIAL FIBRILLATION (AMIODARONE): PREVENTION OF PAROXYSMAL ATRIAL FIBRILLATION,[6] AND HAEMODYNAMICALLY STABLE VENTRICULAR TACHYCARDIA
- 36. CLASS 4 AGENTS CALCIUM CHANNEL BLOCKERS VERAPAMIL DILTIAZEM MECHANISM CALCIUM CHANNEL BLOCKER MEDICAL USES PREVENT RECURRENCE OF PAROXYSMAL SUPRAVENTRICULAR TACHYCARDIA REDUCE VENTRICULAR RATE IN PATIENTS WITH ATRIAL FIBRILLATION
- 37. CLASS 5 Adenosine Digoxin Magnesium sulfate MECHANISM Work by other or unknown mechanisms (direct nodal inhibition) MEDICAL USES Used in supraventricular arrhythmias, especially in heart failure with atrial fibrillation, contraindicated in ventricular arrhythmias. Or in the case of magnesium
- 38. DEFIBRILLATION • DEFIBRILLATION - Is the treatment for immediately life- threatening arrhythmias with which the patient does not have a pulse, ie ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT). • CARDIOVERSION - Is any process that aims to convert an arrhythmia back to sinus
- 39. • Cardioversion is a medical procedure that restores a normal heart rhythm in people with certain types of abnormal heartbeats (arrhythmias). Why it's done • Cardioversion can correct a heartbeat that's too fast (tachycardia) or irregular (fibrillation). Cardioversion is usually used to treat people who have atrial fibrillation or atrial flutter.
- 40. DEFIBRILLATION • DEFIBRILLATION IS DONE AT THE TIME OF EMERGENCY CARDIOVERSION • CARDIOVERSION IS SAME AS DEFIBRILLATION , BUT IT IS PLANNED
- 41. COMPLICATIONS • Dislodged blood clots: Some people who have irregular heartbeats have blood clots in their hearts. Electric Cardioversion can cause these blood clots to move to other parts of your body. This can cause life-threatening complications, such as a stroke or a blood clot traveling to your lungs (pulmonary embolism). • Abnormal heart rhythm: In rare cases, some people who undergo Cardioversion end up with other heart rhythm problems during or after their procedure. This is a rare complication. • Skin burn: Rarely, some people have minor burns on their skin where their
- 42. NURSING DIAGNOSIS: • Knowledge deficit related to cardioversion ( defibrillator) procedure evidenced by frequently questions Objective: • Patient verbalizes the knowledge regarding cardioversion (defibrillation), pre, during and post care after cardioversion Interventions: Followed in the next slides
- 43. NURSING RESPONSIBILITIES BEFORE THE PROCEDURE • Do not allow the patient to eat or drink anything for about 8 hours before your procedure. If medications has to be taken before the procedure, allow him to sip only enough water to swallow the pills. • Before cardioversion, the procedure called a transesophageal echocardiogram (TEE) is done to check for blood clots in the heart, which can be dislodged by cardioversion, causing life-threatening complications • In a transesophageal echocardiogram, throat is numbed and a flexible tube containing a transducer is guided down the throat and into esophagus, which connects the mouth to the stomach. From there, the transducer can obtain more-detailed images of the heart so that your doctor can check for blood clots.
- 44. NURSES RESPONSIBILITY DURING THE PROCEDURE • A nurse will place several large patches called electrodes on the chest. The electrodes will be connected to a cardioversion machine (defibrillator) using wires. • The defibrillator will record the heart rhythm throughout the procedure and will deliver shocks to the heart to restore a normal heart rhythm. This machine can also correct the heart's rhythm if it beats too slowly after cardioversion • Before the shocks are delivered, a nurse will insert an intravenous (IV) line in the arm. The IV line is used to give the medications that will make patient to sleep during the procedure so that patient won't feel any pain from the shocks. the IV line can be used to give additional medications that can help restore the heart rhythm.
- 45. NURSING RESPONSIBILITY AFTER THE PROCEDURE • Electric cardioversion is done on an outpatient basis, meaning patient can go home on the same day procedure is done. Patient will spend an hour or so in a recovery room being closely monitored for complications. •IN CASE OF DEFIBRILLATION ( EMERGENCY ) PATIENT WILL REMAIN IN THE HOSPITAL TILL HE GETS RECOVERED COMPLETELY….
- 46. NURSES RESPONSIBILITIES ( EDUCATION TO THE PATIENT AFTER THE PROCEDURE) • Avoid or limit caffeine and alcohol. • Use less salt (sodium), which can help lower blood pressure. • Increase physical activity. • Quit smoking. • Eat heart-healthy foods and maintain a healthy weight. • Try to limit or manage stress and anger.
- 47. PACEMAKER • A device for stimulating the heart muscle and regulating its contractions. • A pacemaker is a small device with two parts — a generator and wires (leads, or electrodes) — that's placed under the skin in the chest to help control the heartbeat
- 48. WHO NEEDS PACEMAKER •Cardiac arrhythmias •Aging-where heart muscle damage •Some medications- like medicines of cough and cold •Genetic condition which causes the abnormal heart
- 49. WHY ITS DONE • Pacemakers are implanted to help control the heartbeat. They can be implanted temporarily to treat a slow heartbeat after a heart attack, surgery or overdose of medication. • Pacemakers can also be implanted permanently to correct a slow heartbeat (bradycardia) or, in some cases, to help treat heart failure. • Device can be implanted directly into the heart, where it emits an electrical impulse to control the heartbeat.
- 50. WHAT A PACEMAKER DOES • An implanted electronic pacemaker mimics the action of natural pacemaker. An implanted pacemaker consists of two parts: • The pulse generator: This small metal container houses a battery and the electrical circuitry that regulates the rate of electrical pulses sent to heart. • Leads (electrodes). One to three flexible, insulated wires are each placed in a chamber, or chambers, of the heart and deliver the electrical pulses to adjust the heart rate.
- 51. • Pacemakers monitor the heartbeat and, if it's too slow, the pacemaker will speed up your heart rate by sending electrical signals to the heart. In addition, most pacemakers have sensors that detect body motion or breathing rate, which signals the pacemaker to increase the heart rate during exercise to meet body's increased need for blood and oxygen.
- 52. • NURSING DIAGNOSIS: • Knowledge deficit regarding pacemaker evidenced by frequently asked questions • OBJECTIVE: • Patient verbalizes the knowledge regarding the procedure, complications • INTERVENTIONS: • Followed in the next slides
- 53. COMPLICATIONS • Infection where the pacemaker was implanted • Allergic reaction to the dye or anesthesia used during your procedure • Swelling, bruising or bleeding at the generator site • Damage to the blood vessels or nerves near the pacemaker • Collapsed lung
- 54. HOW TO PREPARE THE PATIENT • Electrocardiogram • Holter monitoring. • Echocardiogram. • Stress test
- 55. NURSES RESPONSIBILITY BEFORE THE PROCEDURE •START IV LINE •LOCAL ANESTHESIA •ARRANGEMENT OF SPECIAL EQUIPMENT
- 56. NURSES RESPONSIBILITY DURING THE PROCEDURE • MONITOR VITAL SIGNS
- 57. NURSES RESPONSIBILITY AFTER THE PROCEDURE •Monitor heart rate, rhythm •Pain medication
- 58. SPECIAL INSTRUCTIONS TO THE PATIENT Cellphones: it's safe to talk on a cellphone, but avoid placing the cellphone directly over the pacemaker implantation site when the phone is turned on. Although unlikely, pacemaker could misinterpret the cellphone signal as a heartbeat and withhold pacing, producing symptoms, such as sudden fatigue. Security systems. Passing through an airport metal detector won't interfere with pacemaker, although the metal in it may sound the alarm. But avoid lingering near or leaning against a metal-detection system.
- 59. Medical equipment: • if a doctor is considering any medical procedure that involves intensive exposure to electromagnetic energy, tell him or her that you have a pacemaker. Such procedures include magnetic resonance imaging, therapeutic radiation for cancer treatment and shock wave lithotripsy, which uses shock waves to break up large kidney stones or gallstones. POWER GENERATING EQUIPMENT: • Stand at least 2 feet (60 centimeters) from welding equipment, high-voltage transformers or motor-generator systems. If the patient work around such equipment, doctor can arrange a test in the workplace to determine whether it affects the pacemaker.
- 60. NURSING INTERVENTION FOR DYSRHYTHMIAS ( ARRHYTHMIAS) Nursing diagnosis: • Chest discomfort/chest pain secondary to cardiac dysrhythmias associated with altered myocardial automaticity, conductivity or contractibility Objective: Reduce chest discomfort/pain Interventions: Assess for signs of ineffective perfusion by system Renal: oliguria, anuria Gastrointestinal: nausea, hypoactive or absent bowel sounds
- 61. • Peripheral: Odema, altered skin colour, temperature, sensation or integrity, weak or absent pulse • Cerebral: dizziness, altered mental status, confusion, anxiety, syncope, altered pupillary response, speech abnormality • Cardiopulmonary: Hypotension, abnormal respiratory rate, capillary refill more than 3 seconds, chest pain, dyspnea, crackles and wheezes, jugular vein distention • Intervention: • Assess for and report signs/symptoms of cardiac dysrhythmias (e.g. irregular apical pulse, adult pulse rate below 60 or above 100 beats/minute, apical-radial pulse deficit, syncope, palpitations).
- 62. Reduce cardiac workload • Position patient to minimizes discomfort and facilitate respiration. • Minimize anxiety with calm reassurance and education. • Communicate rationale for monitoring and treatments. • Discuss the benefits calm with the patient and family. Initiate EKG monitor and pulse oximetry per policy. IV access, O2, medication and 12 lead-EKG as ordered, monitor vital signs. • Positive inotropic agents (e.g. dobutamine, dopamine) to increase myocardial contractility • Vasodilators (e.g. nitroglycerin) to decrease cardiac workload • ACE inhibitors (e.g. captopril, ramipril) to decrease cardiac workload • Diuretics for elevated capillary wedge pressure • Morphine sulfate to reduce pain, preload and anxiety.
- 63. Anticipate the need to initiate cardiopulmonary resuscitation. Assess for contributing factors: pain, fluid and electrolyte imbalance, drug toxicity (especially digoxin), medication non- adherence. Provide psychosocial support for patient and family members. • If the dysrhythmia is a life-threatening type, encourage the family unit to calmly formulate a plan of action. • Reassure the patient will receive the best care in keeping with his written directives or medical power of attorney. • Communicate the availability and value of social services as