1. The document describes various types of pain that can occur with complete dentures, including localized, generalized, and diffuse pain.
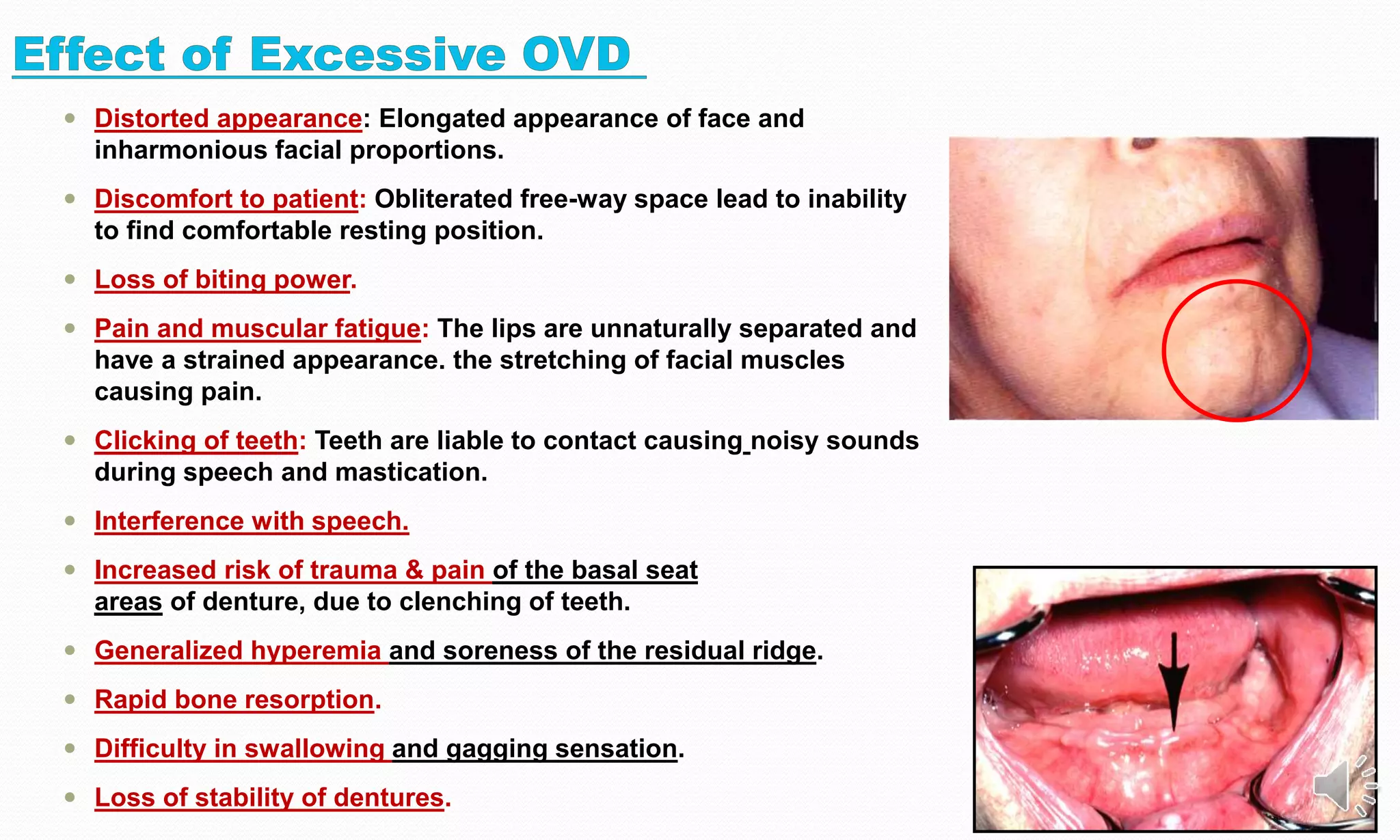
2. Common causes of denture pain are incorrect vertical dimension, improper tooth positioning, and occlusal discrepancies.
3. Treatment involves identifying the specific error, such as reducing vertical dimension for high bite, and remaking or adjusting the dentures.