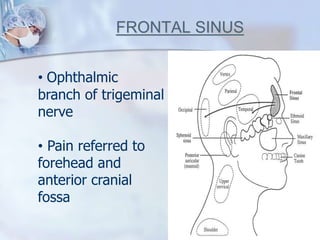
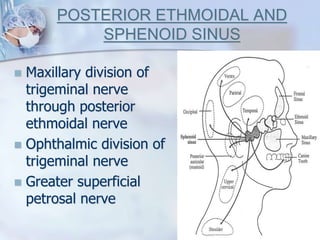
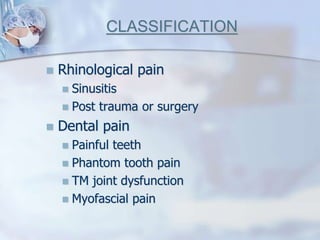
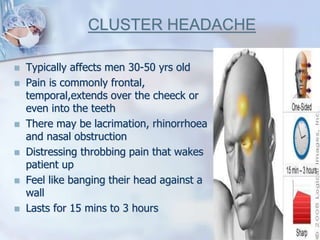
This document discusses the evaluation and classification of facial pain and headache. It notes that while patients are often referred for suspected sinusitis, few actually have sinogenic pain. A thorough history is key to determining the cause, such as determining if the pain is continuous or intermittent, any precipitating or relieving factors, and the effect on daily life. Common etiologies include sinusitis, dental issues, trigeminal neuralgia, migraine, tension headaches, and atypical facial pain. A neurological examination and imaging may aid diagnosis. Proper classification is important for determining appropriate treatment.