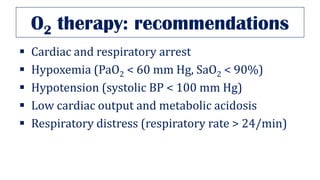
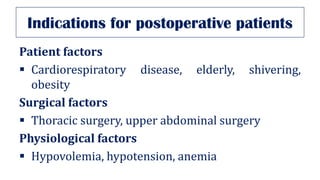
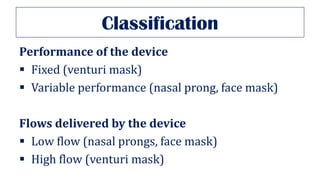
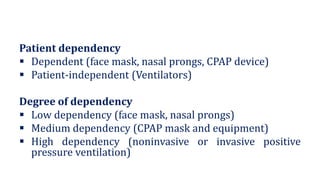
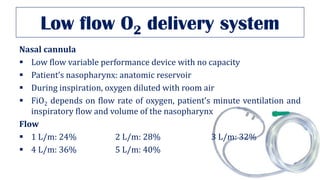
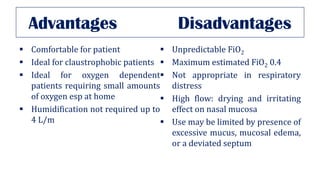
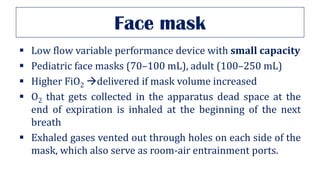
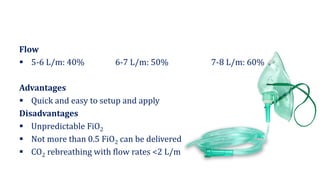
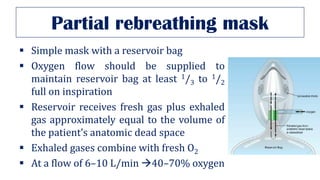
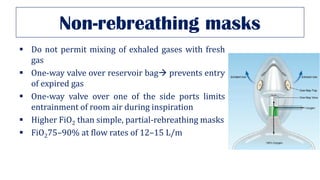
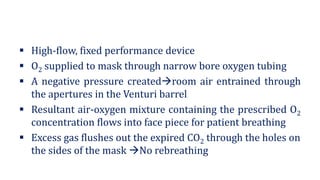
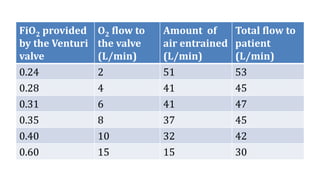
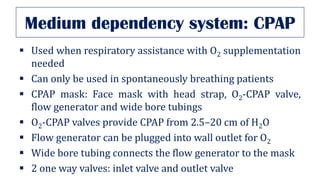
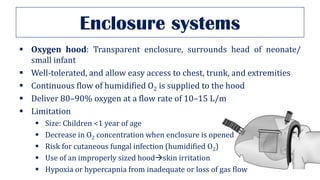
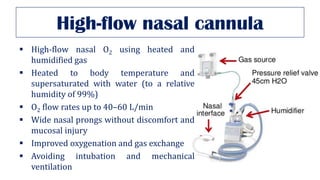
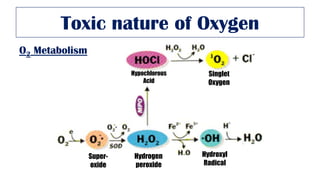
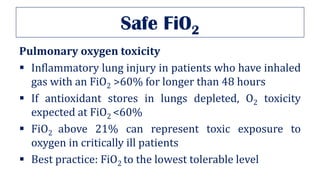
This document discusses oxygen therapy and different oxygen delivery systems. It begins by introducing the history and indications for oxygen therapy. It then categorizes oxygen delivery systems based on their performance, flows delivered, patient dependency, and degree of dependency. The document goes on to describe specific low flow systems like nasal cannula and face masks. It also covers high flow systems like venturi masks, CPAP, and high flow nasal cannulas. Finally, it discusses the toxic effects of prolonged high concentration oxygen therapy.