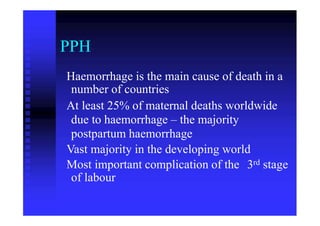
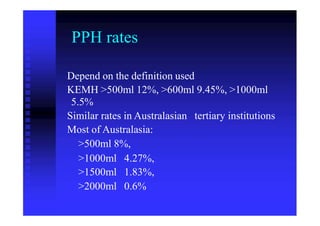
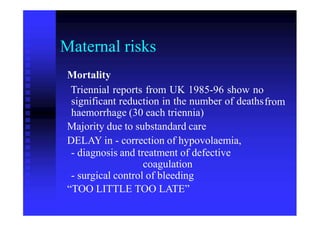
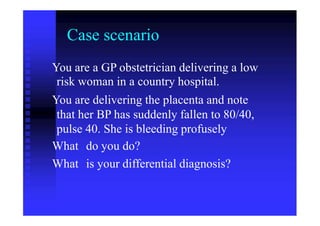
This document discusses post-partum hemorrhage (PPH), including its definition, causes, risk factors, prevention, and management. It describes:
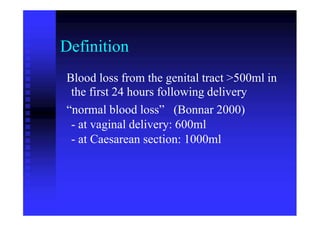
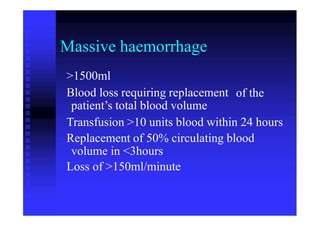
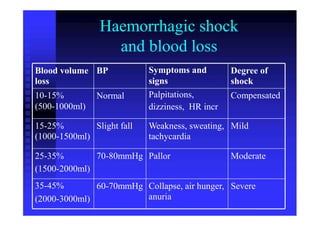
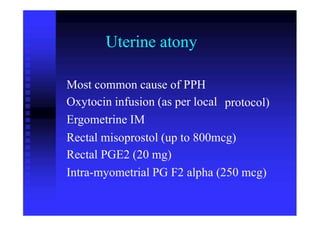
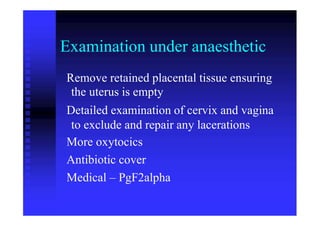
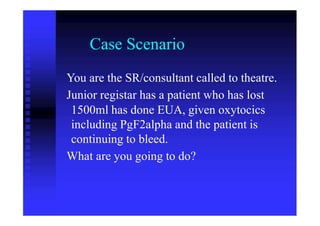
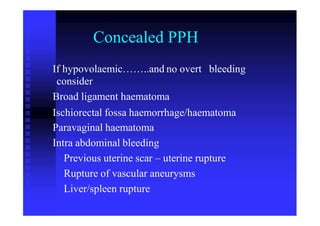
1) PPH is defined as blood loss over 500ml within 24 hours of delivery. The main cause is uterine atony but can also be due to retained placenta or trauma.
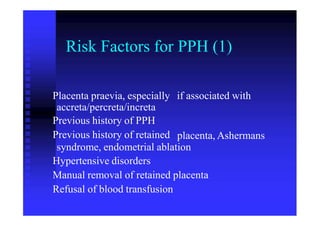
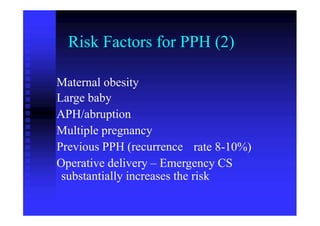
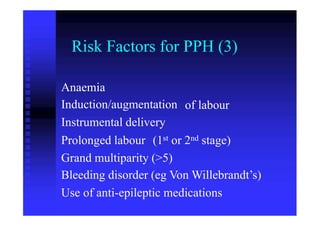
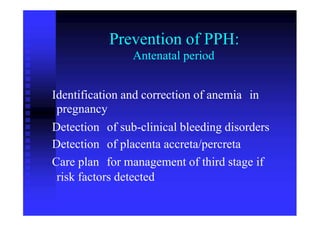
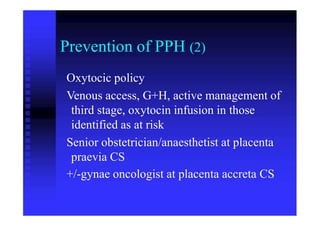
2) Risk factors include previous c-section, large babies, and medical conditions like placenta previa. Prevention focuses on identifying risks antenatally and using oxytocics to manage the third stage of labor.
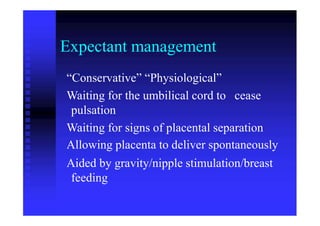
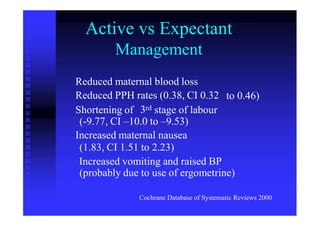
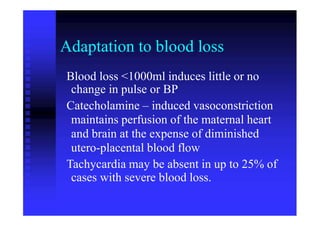
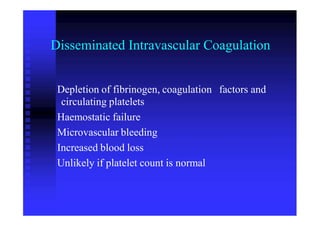
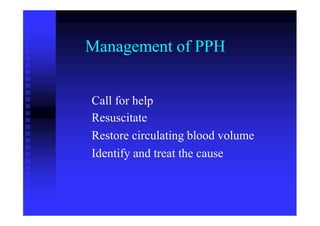
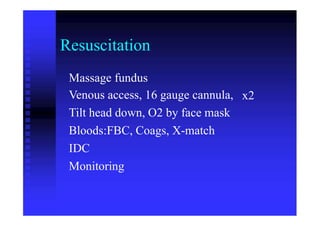
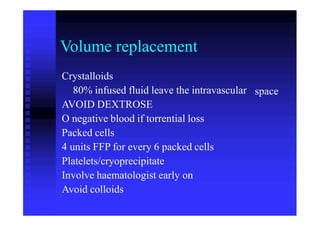
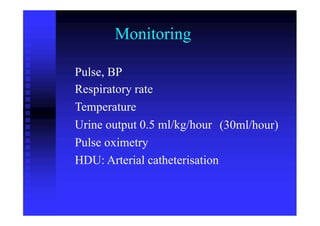
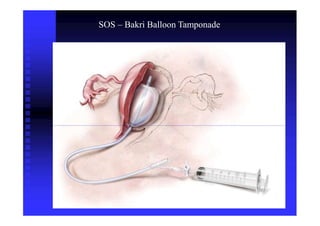
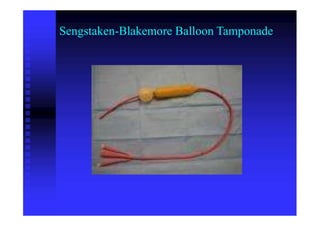
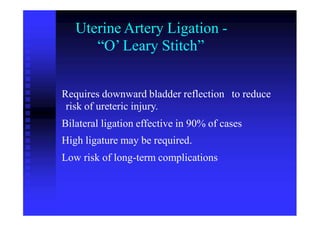
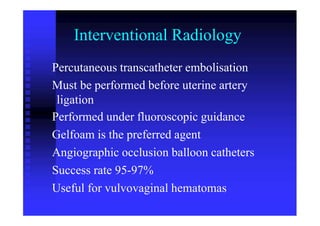
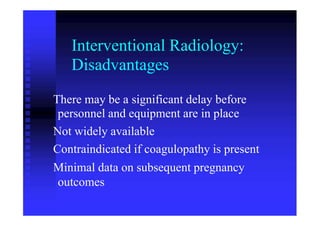
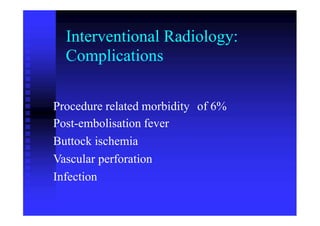
3) Initial management of PPH involves resuscitation, oxytocics, and identifying the cause. Further steps may include balloon