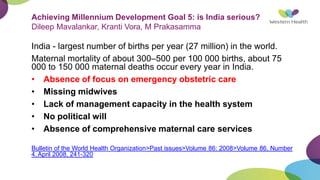
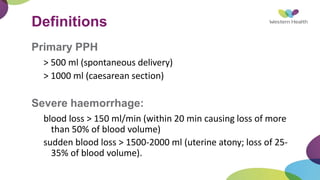
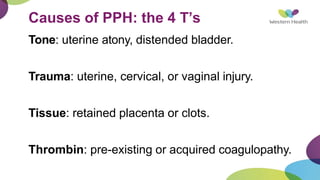
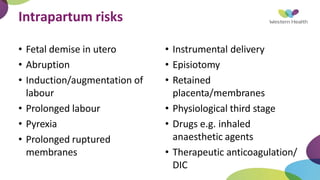
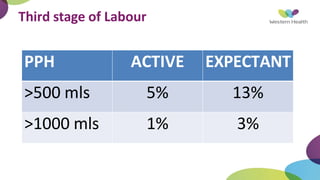
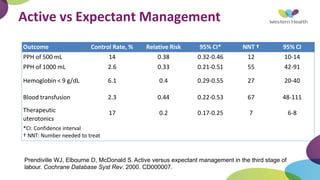
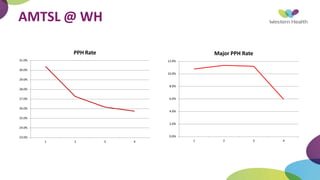
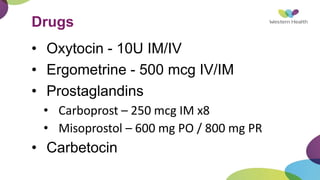
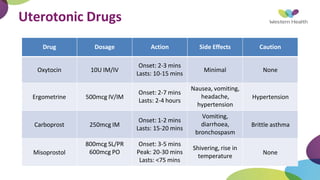
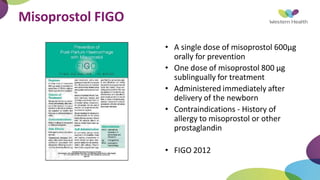
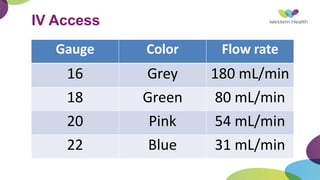
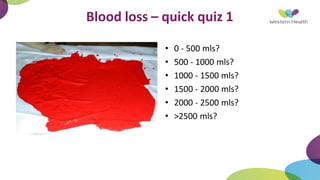
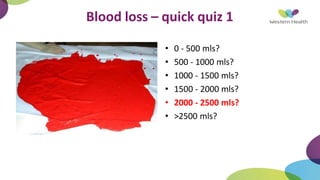
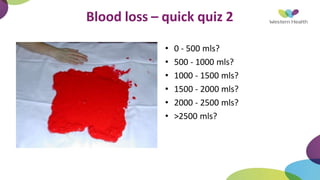
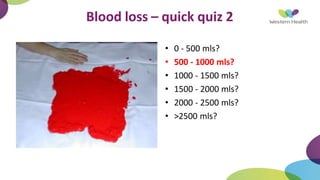
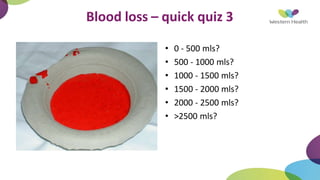
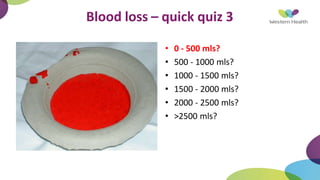
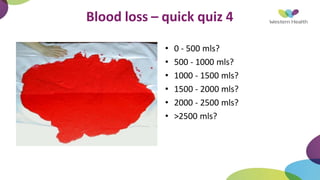
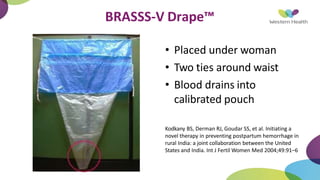
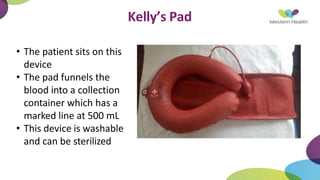
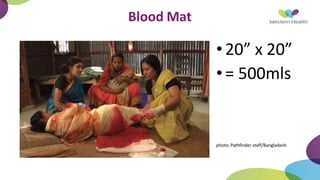
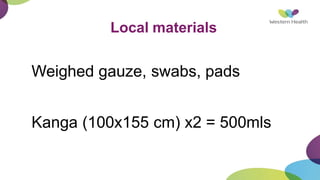
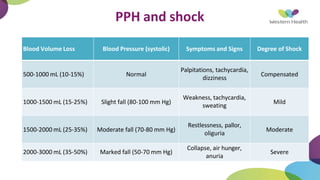
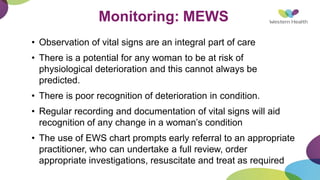
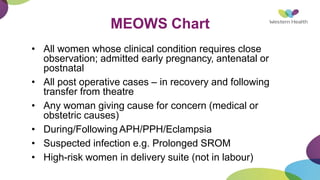
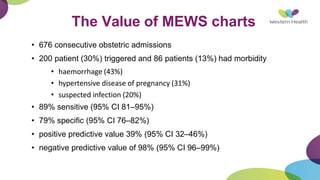
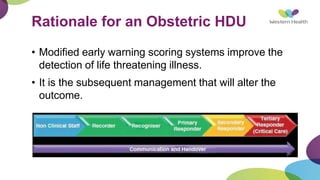
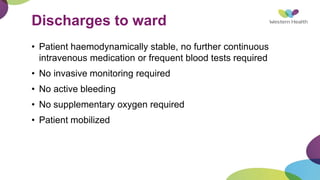
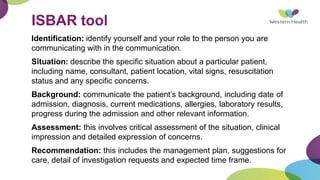
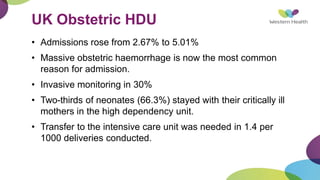
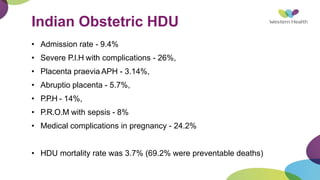
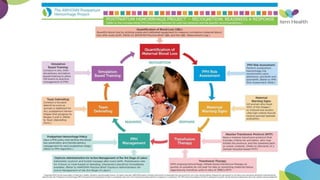
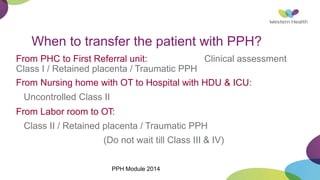
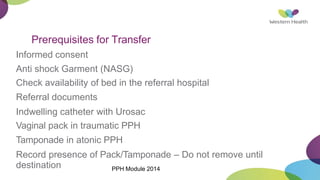
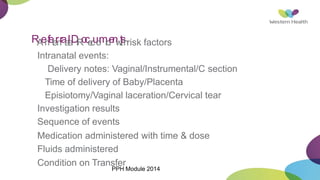
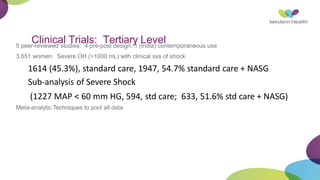
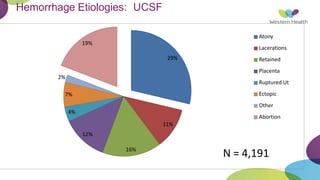
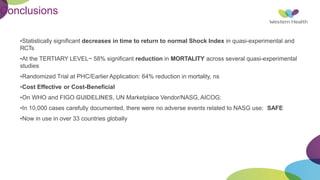
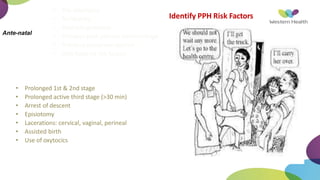
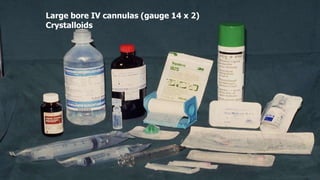
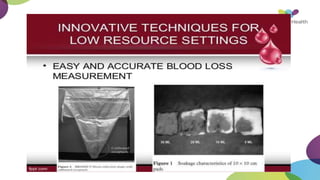
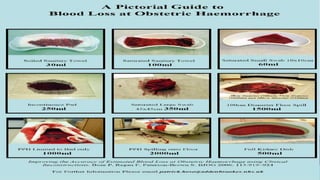
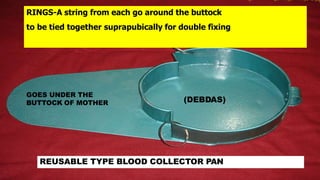
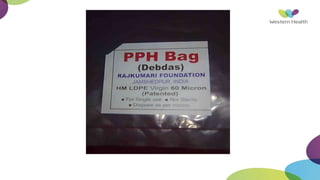
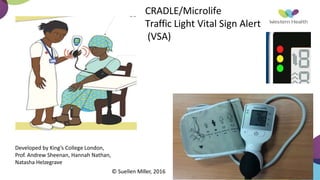
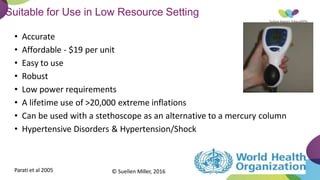
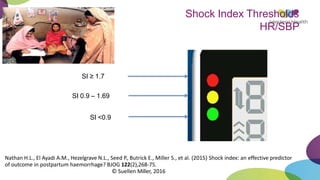
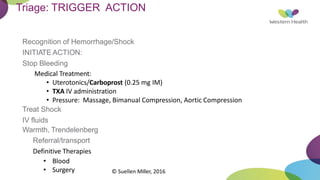
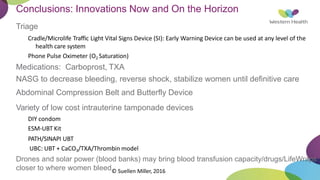
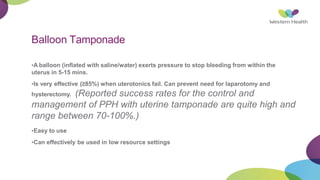
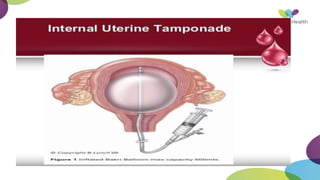
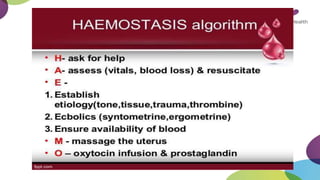
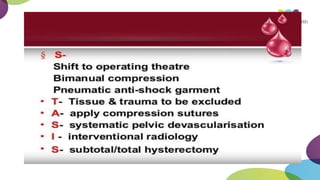
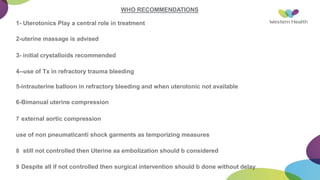
This document summarizes obstetric drills on PPH (postpartum hemorrhage) that took place in six major cities in India from August 2016. It provides details on the trainers and hospitals that conducted hands-on training over six days. The document then discusses definitions and causes of PPH, risk factors, management including uterotonic drugs and IV fluids, techniques for estimating blood loss, use of monitoring like MEOWS (maternal early warning systems) to identify deterioration, and importance of timely response to prevent shock.