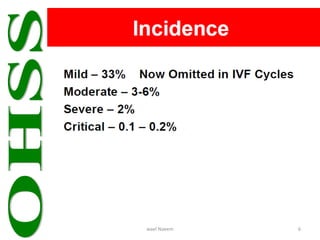
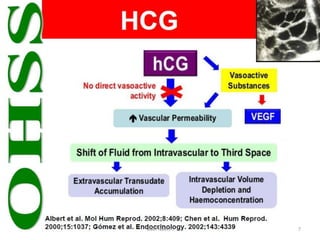
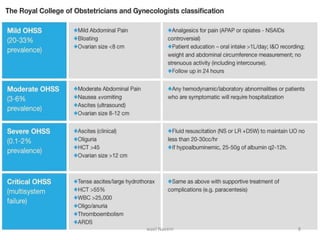
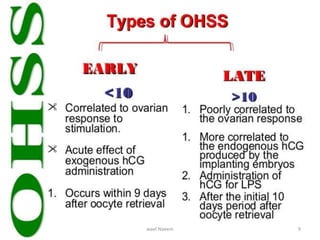
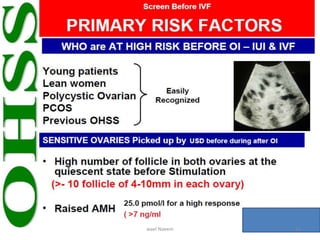
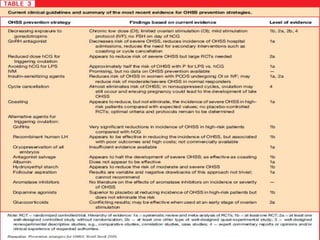
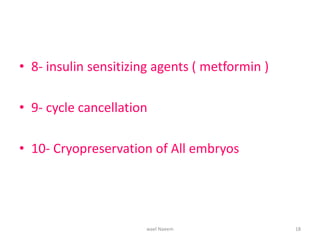
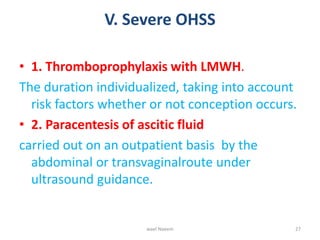
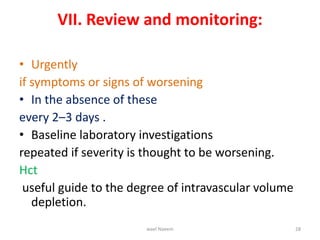
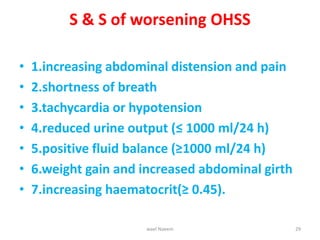
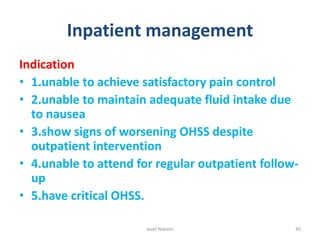
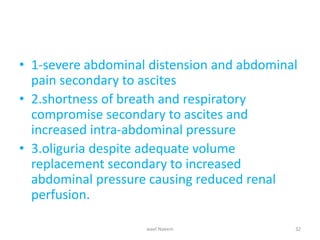
This document discusses the management of ovarian hyperstimulation syndrome (OHSS). It covers the background, pathophysiology, clinical presentations, complications, prevention, and treatment of OHSS. Prevention strategies include reducing gonadotropin doses, using GnRH antagonists, reducing or avoiding HCG, cycle cancellation, and cryopreservation of embryos. Treatment involves reassurance, fluid management, analgesia, thromboembolism prophylaxis, and paracentesis for ascites. Hospitalization is required for uncontrolled pain, inability to maintain fluids, or worsening signs like shortness of breath.