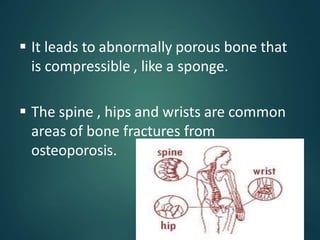
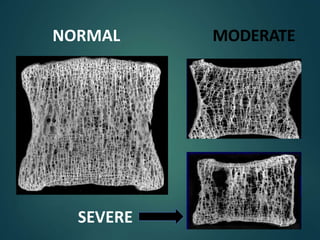
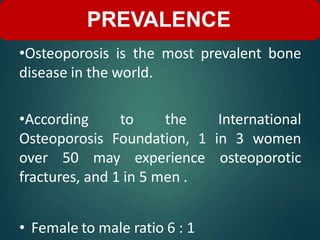
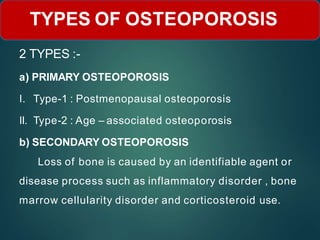
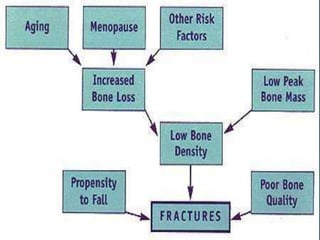
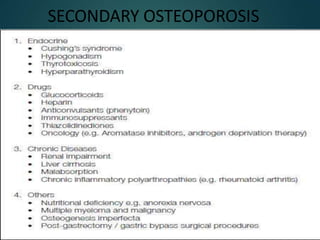
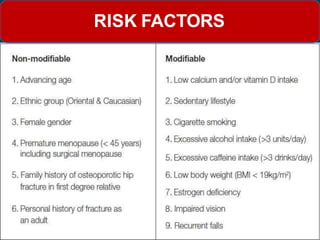
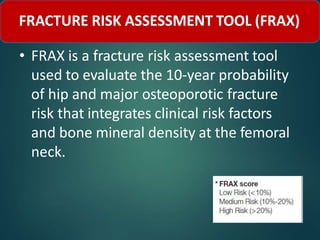
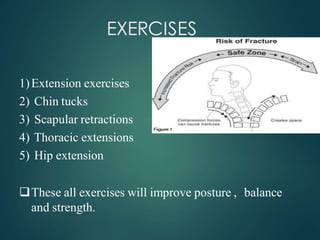
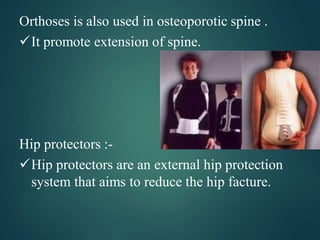
Osteoporosis is a disease characterized by low bone mass and deterioration of bone tissue, leading to fragile bones and increased risk of fractures. It is most common in postmenopausal women and older adults. Physiotherapy management focuses on exercises to improve posture, balance, strength, flexibility, and weight bearing through the bones to help prevent fractures and bone loss. Lifestyle factors like diet, calcium supplementation, and avoiding risk factors can also help to manage osteoporosis.