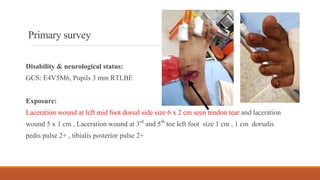
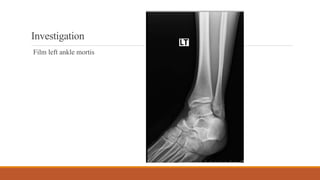
- A 16-year-old Thai man presented to the emergency room with a laceration wound on his left foot after falling off his motorcycle. On examination, he had a 6x2 cm laceration wound on his left midfoot with tendon tearing and smaller wounds on his toes. X-rays showed an open fracture of the tarsal bone.
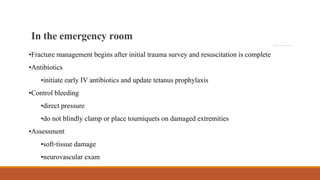
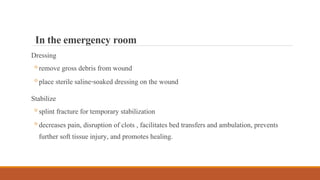
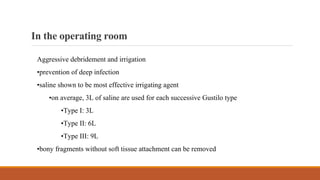
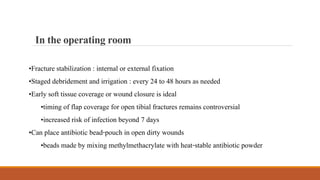
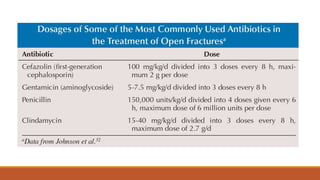
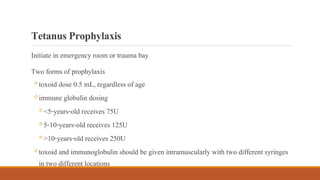
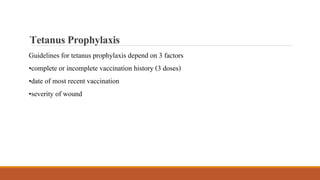
- In the emergency room, the wounds were irrigated and dressed. IV antibiotics and tetanus prophylaxis were started. In the operating room, the wounds underwent aggressive debridement and irrigation. The fractures were stabilized with internal fixation. Staged debridements were planned every 24-48 hours as needed.
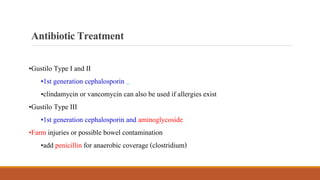
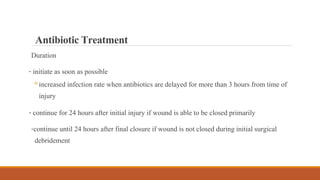
- Open fractures require prompt antibiotic treatment