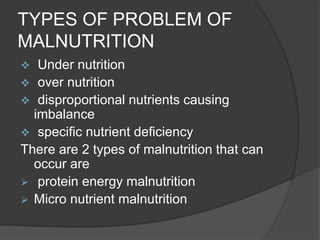
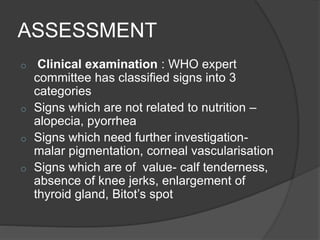
Malnutrition is caused by relative or absolute deficiency or excess of nutrients and can manifest as undernutrition or overnutrition. The main types of undernutrition are protein-energy malnutrition (PEM), which includes kwashiorkor and marasmus, and micronutrient malnutrition. PEM is caused by inadequate intake of proteins or calories and results in edema, wasting, and other signs. Micronutrient deficiencies can result in conditions like night blindness, anemia, and neurological impairments. Malnutrition has multiple causes including poverty, diseases, customs, and lack of knowledge. It is assessed using tools like growth charts, biochemical tests, and morbidity rates. Prevention focuses on identification, feeding programs, education, and increasing access to nutrit
![TYPES OF
MALNUTRITION A] protein energy malnutrition: 2 types
Kwashiorkor Marasmus
Due to decreased intake due to decreased
of proteins. Intake of calories.
clinical features
edema in lower leg, face loss of subcuta-
& lower arms. neous fat.
Irritabilty Muscle wasting](https://image.slidesharecdn.com/malnutrition-170628061653/85/Malnutrition-8-320.jpg)
![B] MICRONUTRIENT
MALNUTRITION
Deficiency of vitamins & minerals
deficiency of vitamin A
night blindness
conjuctival xerosis
bitot’s spots
corneal xerosis
keratomalacia](https://image.slidesharecdn.com/malnutrition-170628061653/85/Malnutrition-11-320.jpg)