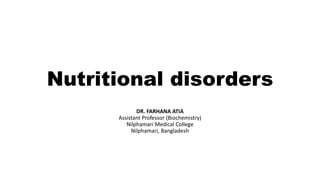
This document discusses various nutritional disorders including malnutrition, undernutrition, micronutrient deficiencies, overweight, obesity, and metabolic syndrome. It defines each condition and provides details on signs, causes, and health effects. Malnutrition refers to deficiencies or imbalances in energy and nutrient intake and includes undernutrition, micronutrient deficiencies, overweight, and obesity. Undernutrition is insufficient food intake over time and includes wasting, stunting, and being underweight. Micronutrient deficiencies involve inadequate intake of vitamins and minerals. Overweight and obesity result from excessive calorie intake over time and not enough physical activity.





![Malnutrition in Bangladesh
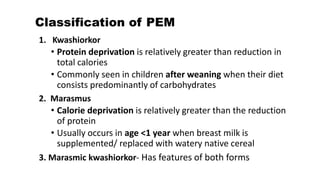
• PEM [Protein energy malnutrition]
• Iron deficiency
• Vitamin A deficiency
• Iodine deficiency (Endemic goiter)
• Zinc deficiency
• Vit-B12 & Folic acid deficiency (combined deficiency
anemia)
• Diabetes & cardiovascular disease
• Malnutrition due to illiteracy & ignorance](https://image.slidesharecdn.com/nutritionaldisorders-200919141012/85/Nutritional-disorders-7-320.jpg)