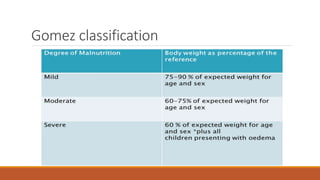
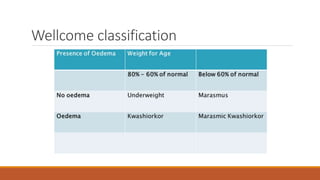
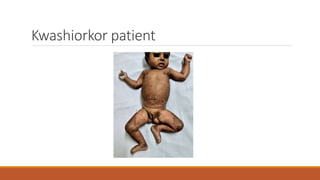
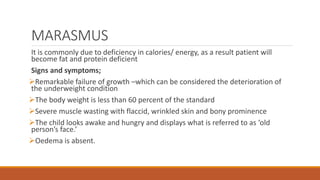
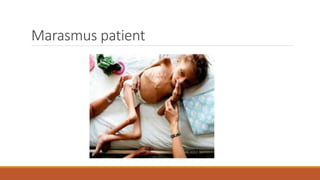
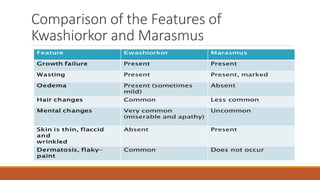
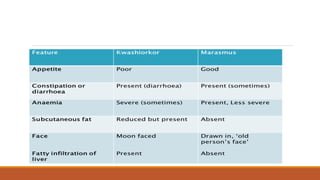
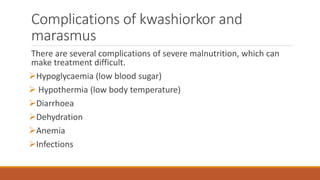
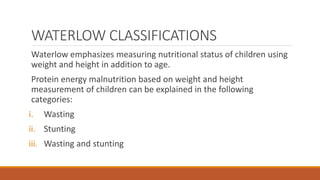
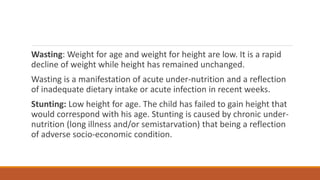
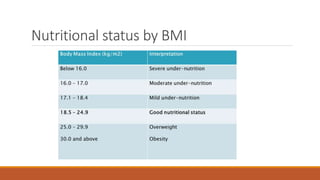
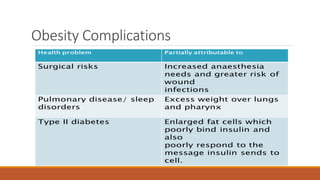
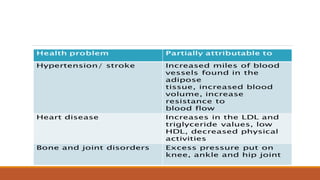
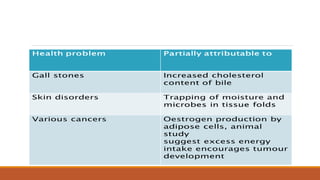
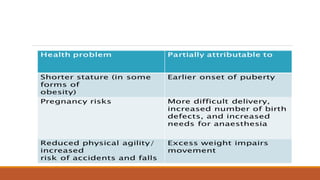
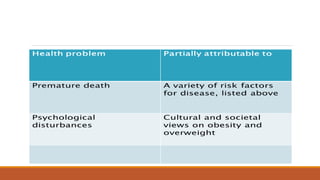
The document discusses protein energy malnutrition (PEM), highlighting its classifications (Gomez, Wellcome, and Waterlow), causes, and symptoms including underweight, kwashiorkor, and marasmus, particularly in infants and children. It emphasizes the complexities in preventing PEM and outlines obesity's definition, causes, classifications, and health risks, as well as limitations of BMI for assessing nutritional status. Both conditions are linked to significant health complications and require comprehensive strategies for prevention and management.