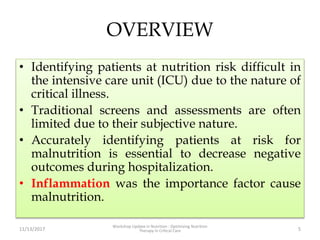
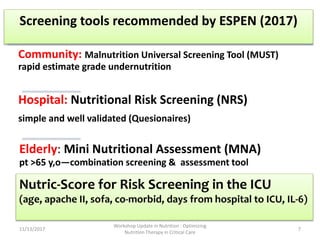
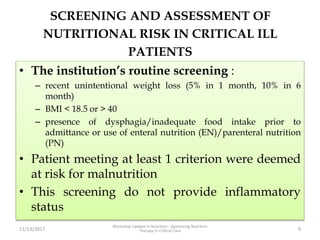
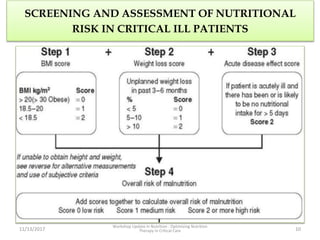
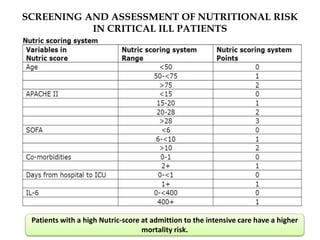
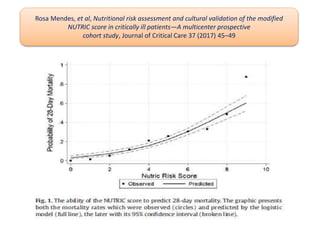
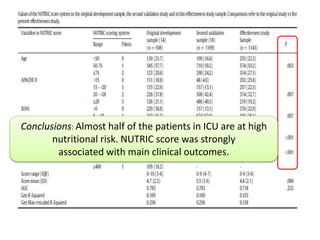
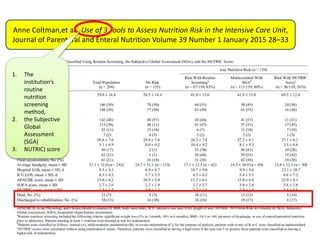
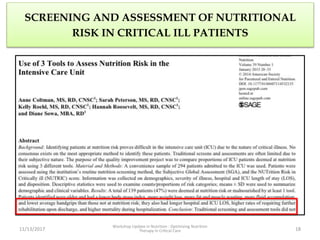
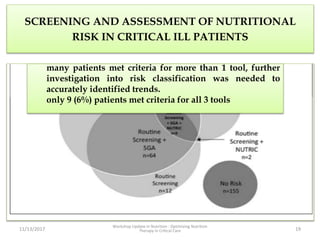
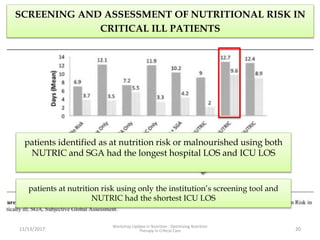
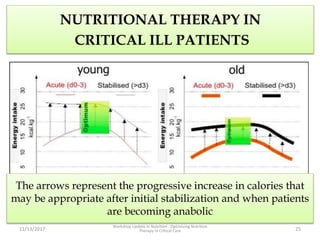
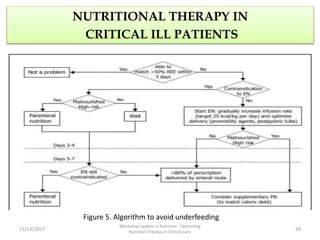
This document outlines the roles and qualifications of a senior lecturer in nutrition, highlighting various aspects of nutritional assessment and therapy in critically ill patients. It discusses the significance of accurate nutritional screening tools, such as the nutric score and subjective global assessment, to identify malnutrition risk in the ICU. The document also addresses the challenges and guidelines for nutritional therapy in critical care settings, emphasizing the importance of tailored nutritional support for improving patient outcomes.