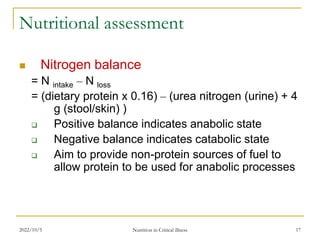
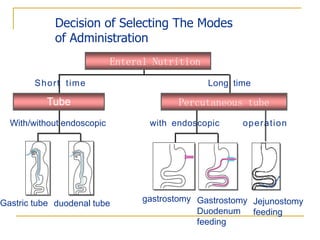
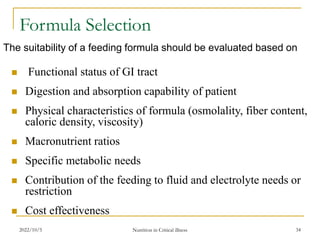
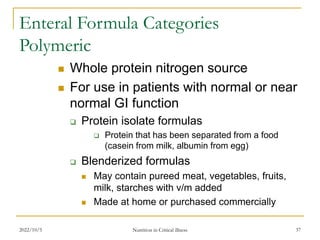
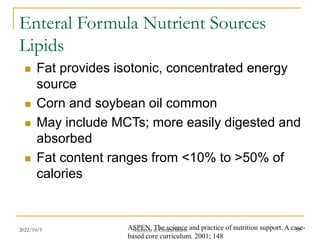
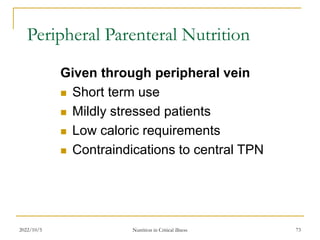
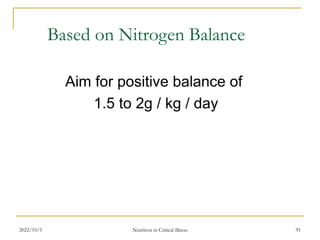
This document discusses nutritional support in critical illness. It defines nutritional support as the provision of nutrients to patients who cannot meet their nutritional needs through standard diets. Malnutrition occurs in approximately 40% of hospitalized patients and can lead to increased morbidity and mortality by impairing organ function and healing. The document outlines the history of nutritional support, from overfeeding in the 1970s to more targeted support today. It discusses screening patients for nutritional risk and assessing nutritional status. The key questions of who needs support, when to start, how much to provide, and how to provide it are addressed. Enteral nutrition is generally preferred over parenteral nutrition. The document describes different enteral feeding methods and formulas for meeting various nutritional needs.