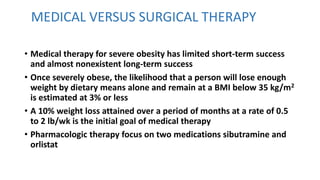
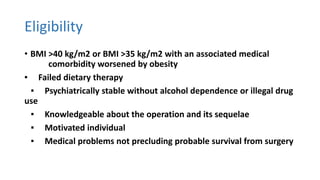
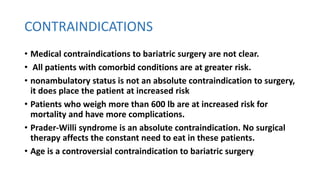
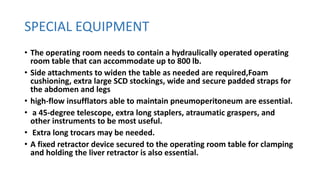
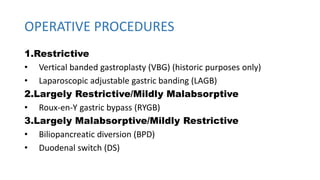
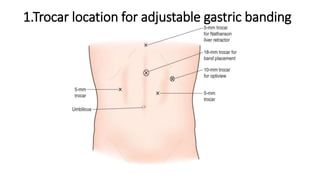
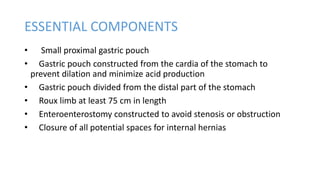
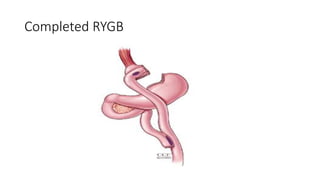
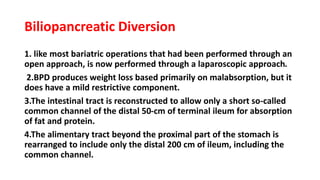
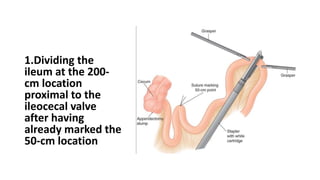
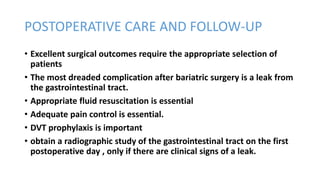
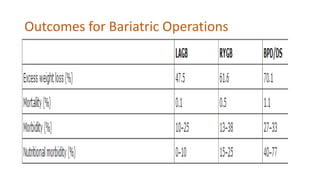
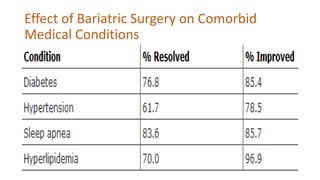
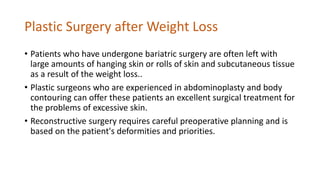
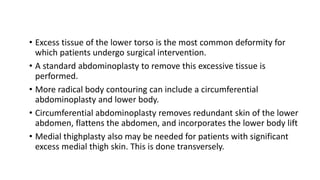
Bariatric surgery is effective for treating morbid obesity. Common procedures include gastric bypass and gastric banding, which achieve weight loss through restriction and malabsorption. Candidates must have a BMI over 40 or over 35 with comorbidities. Risks include leaks and DVTs. Weight loss improves related conditions like diabetes. Plastic surgery after significant weight loss addresses excess skin.