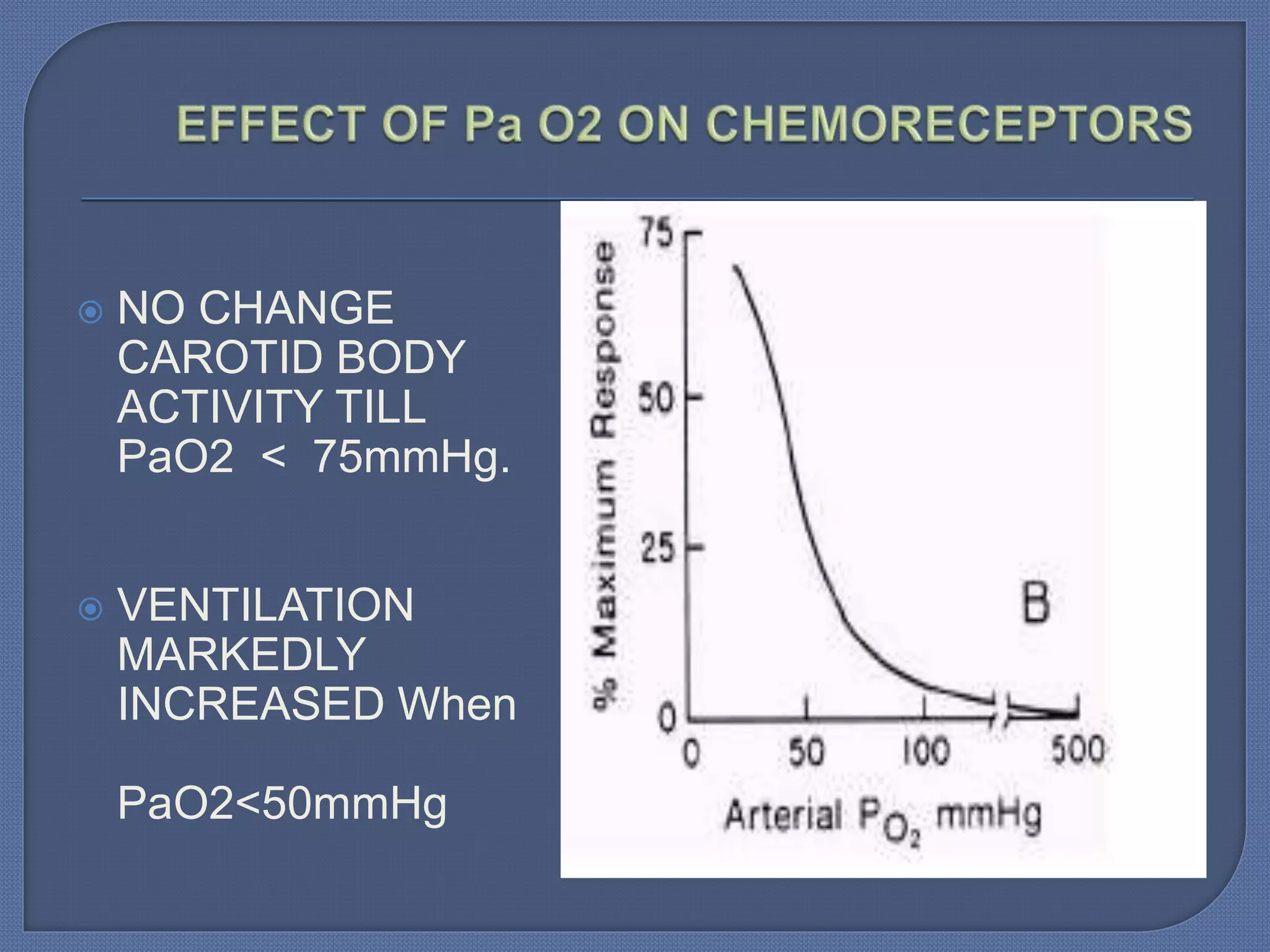
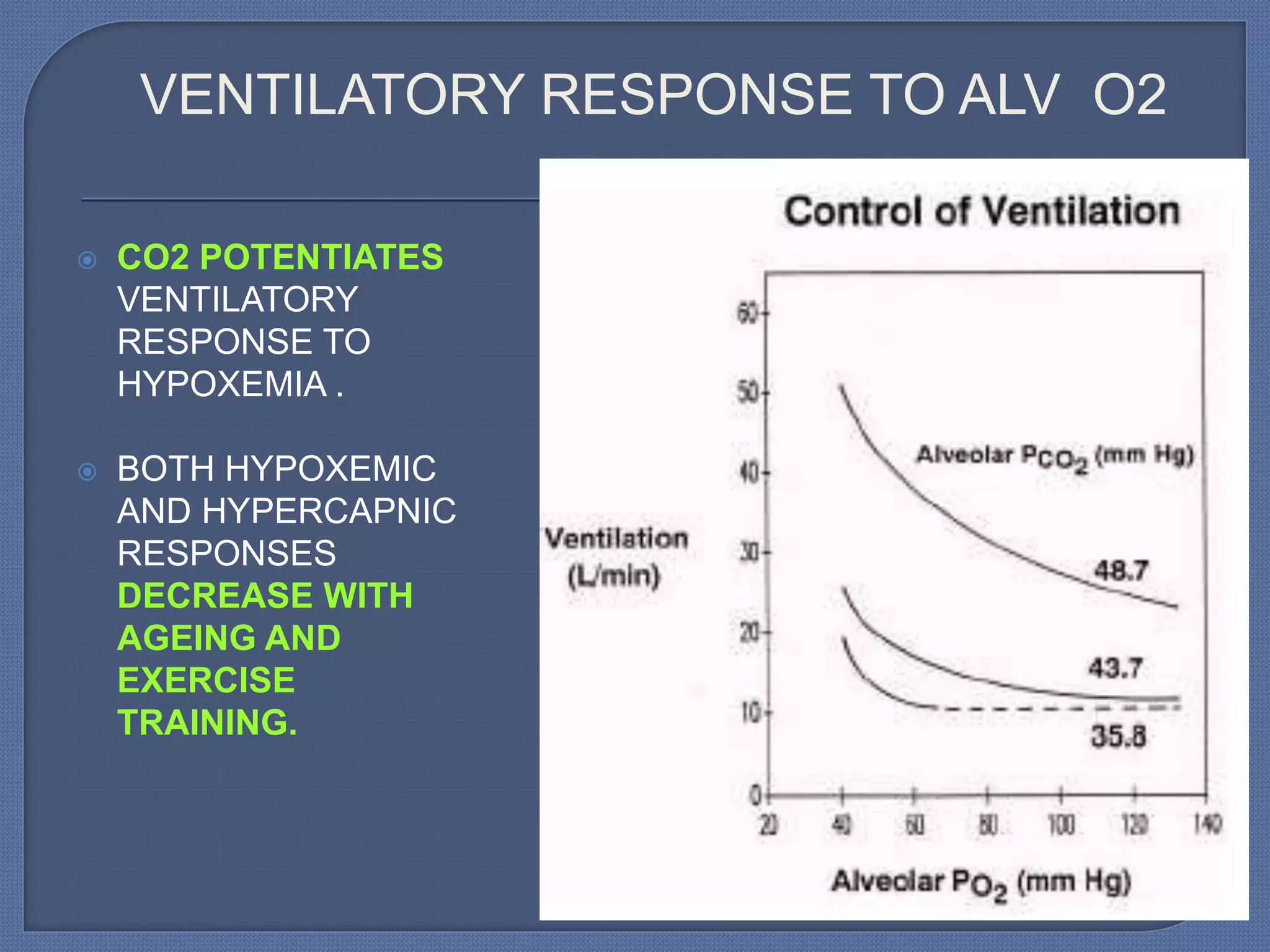
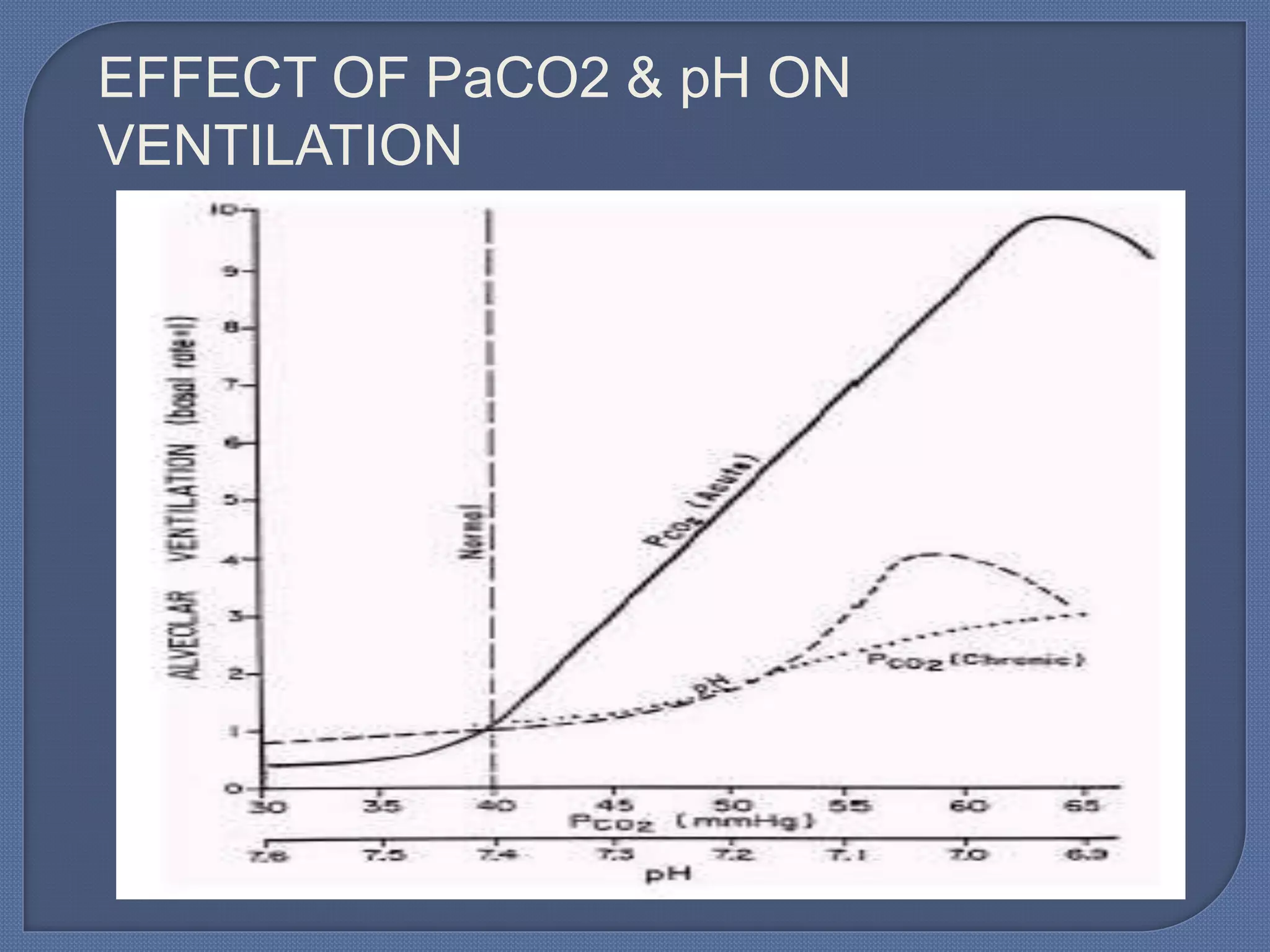
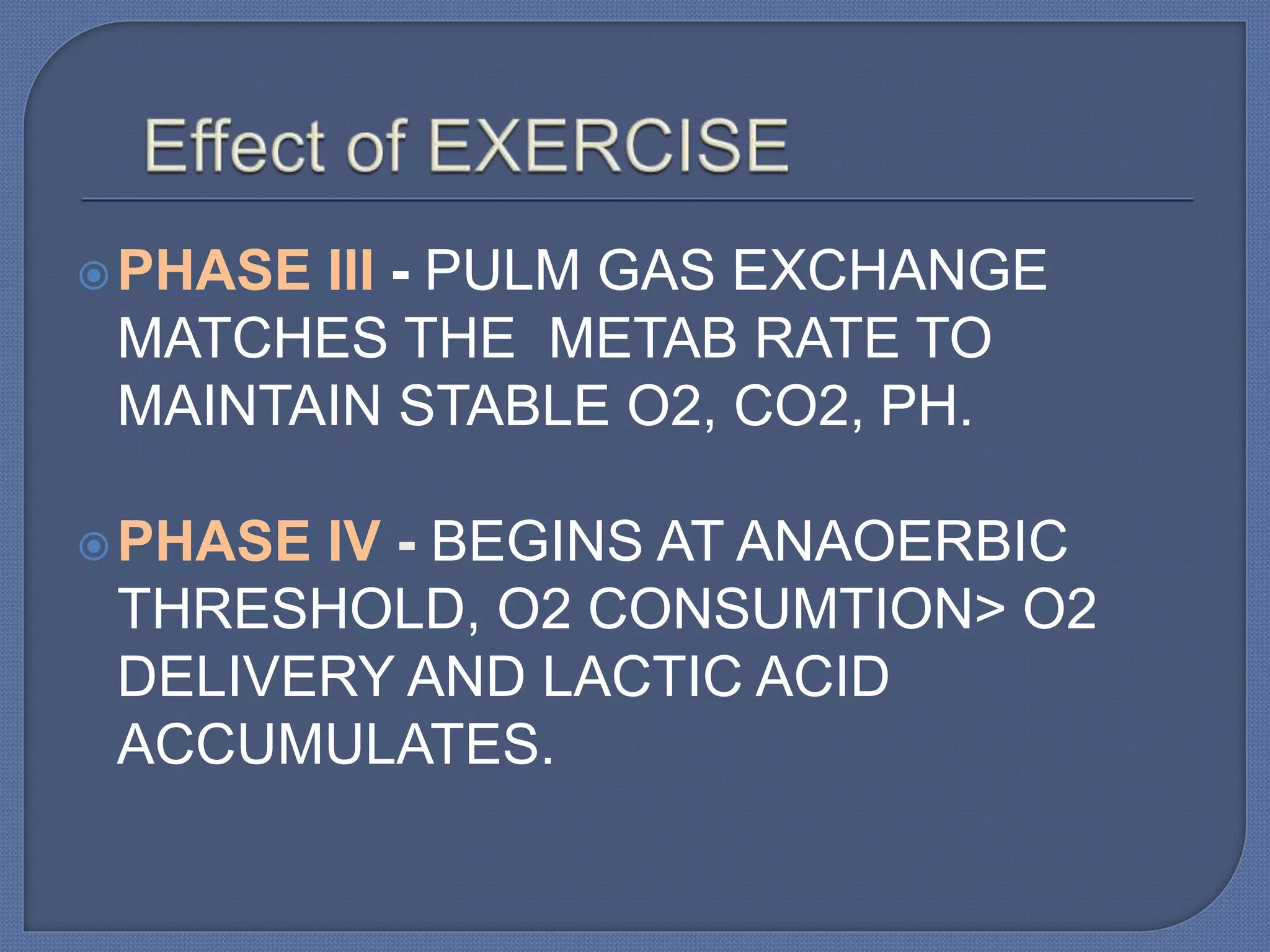
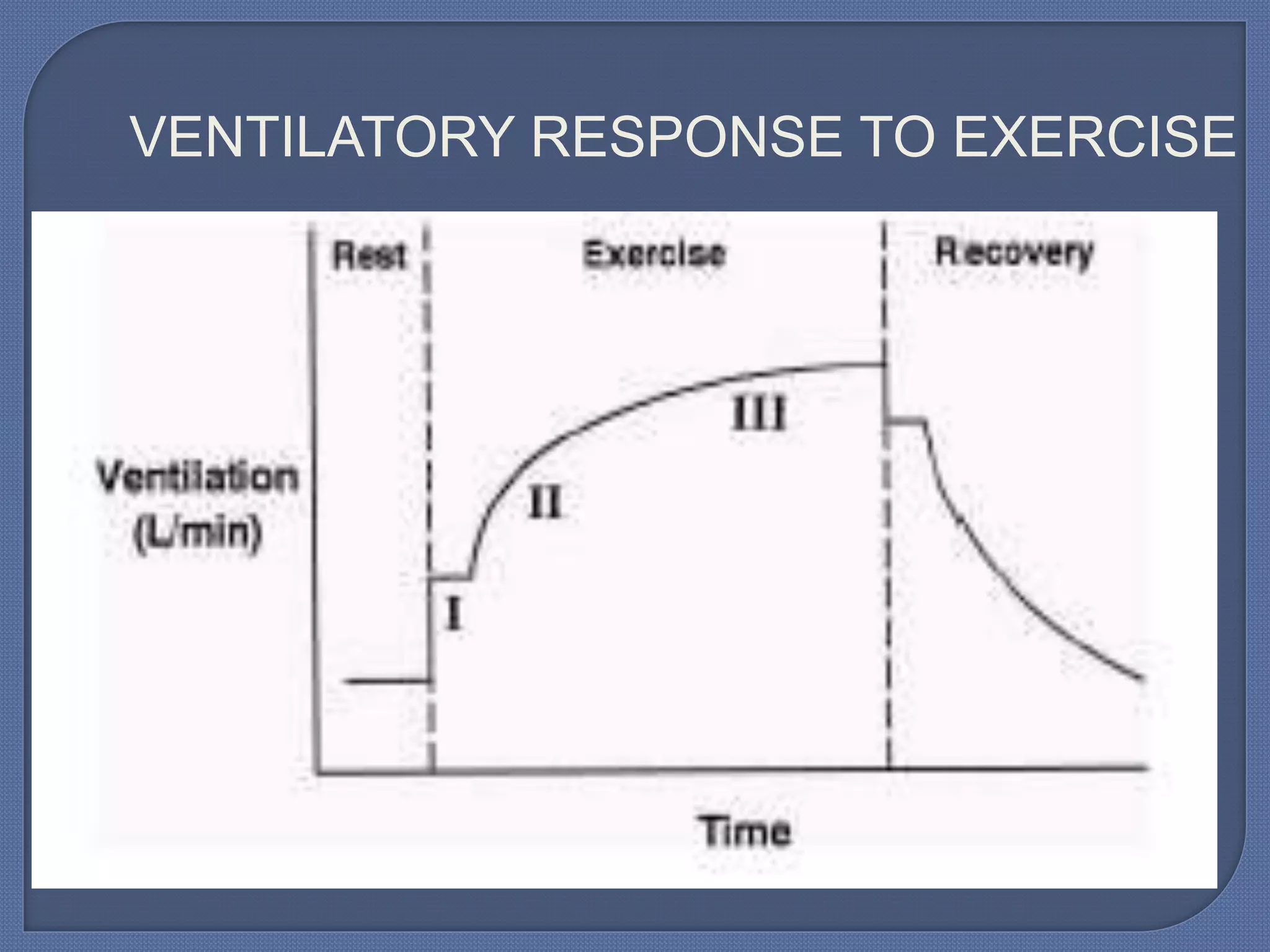
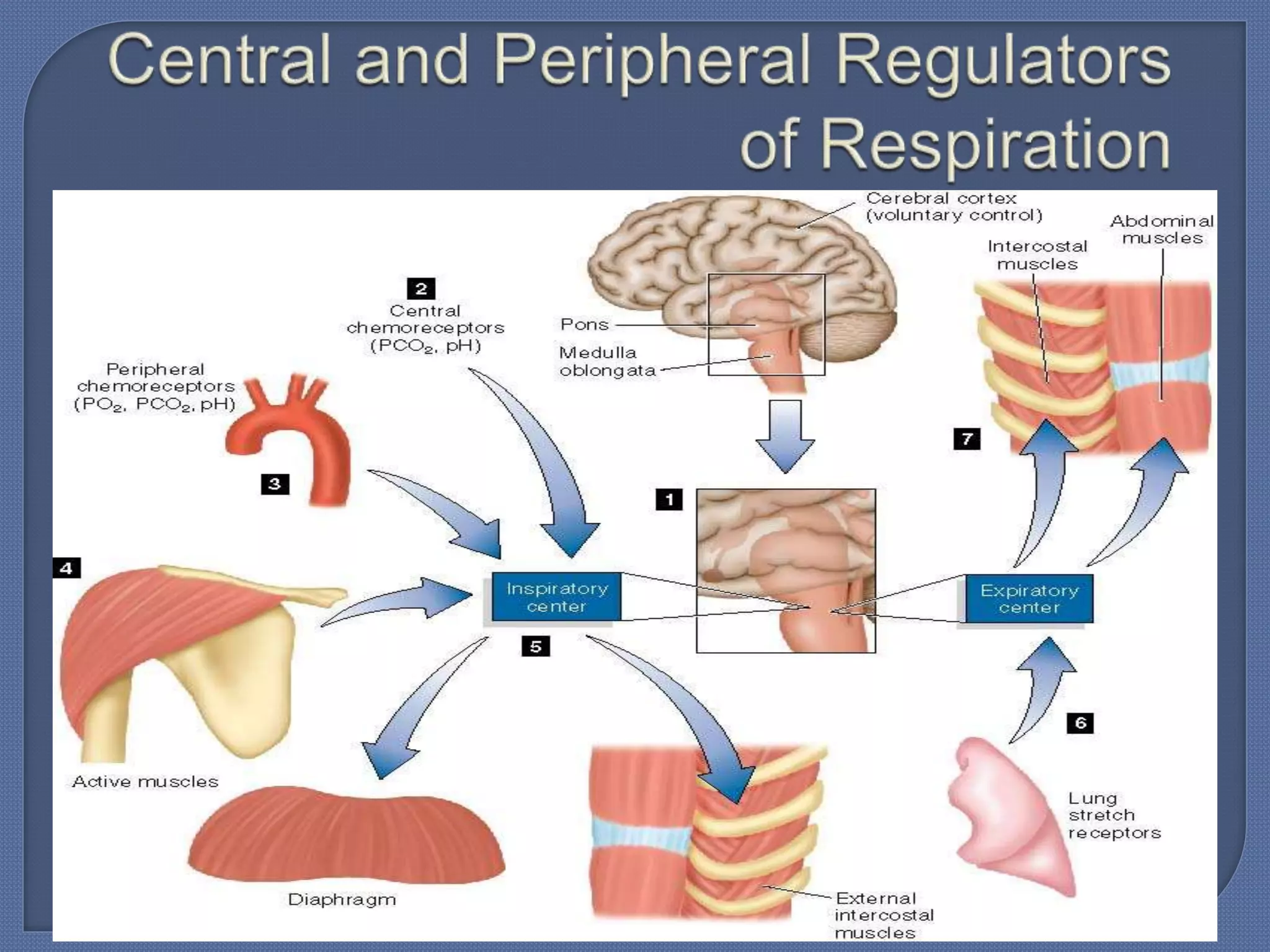
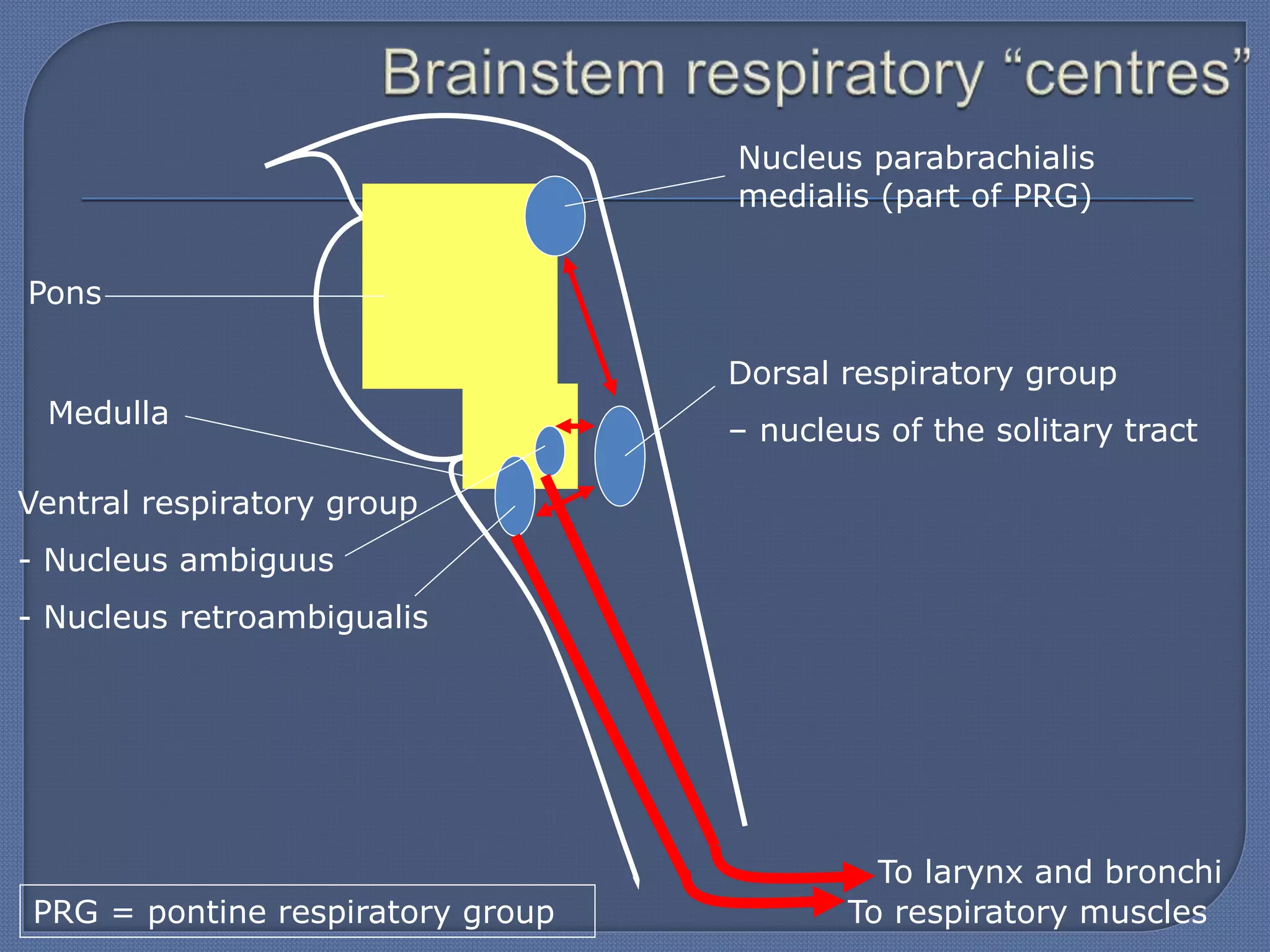
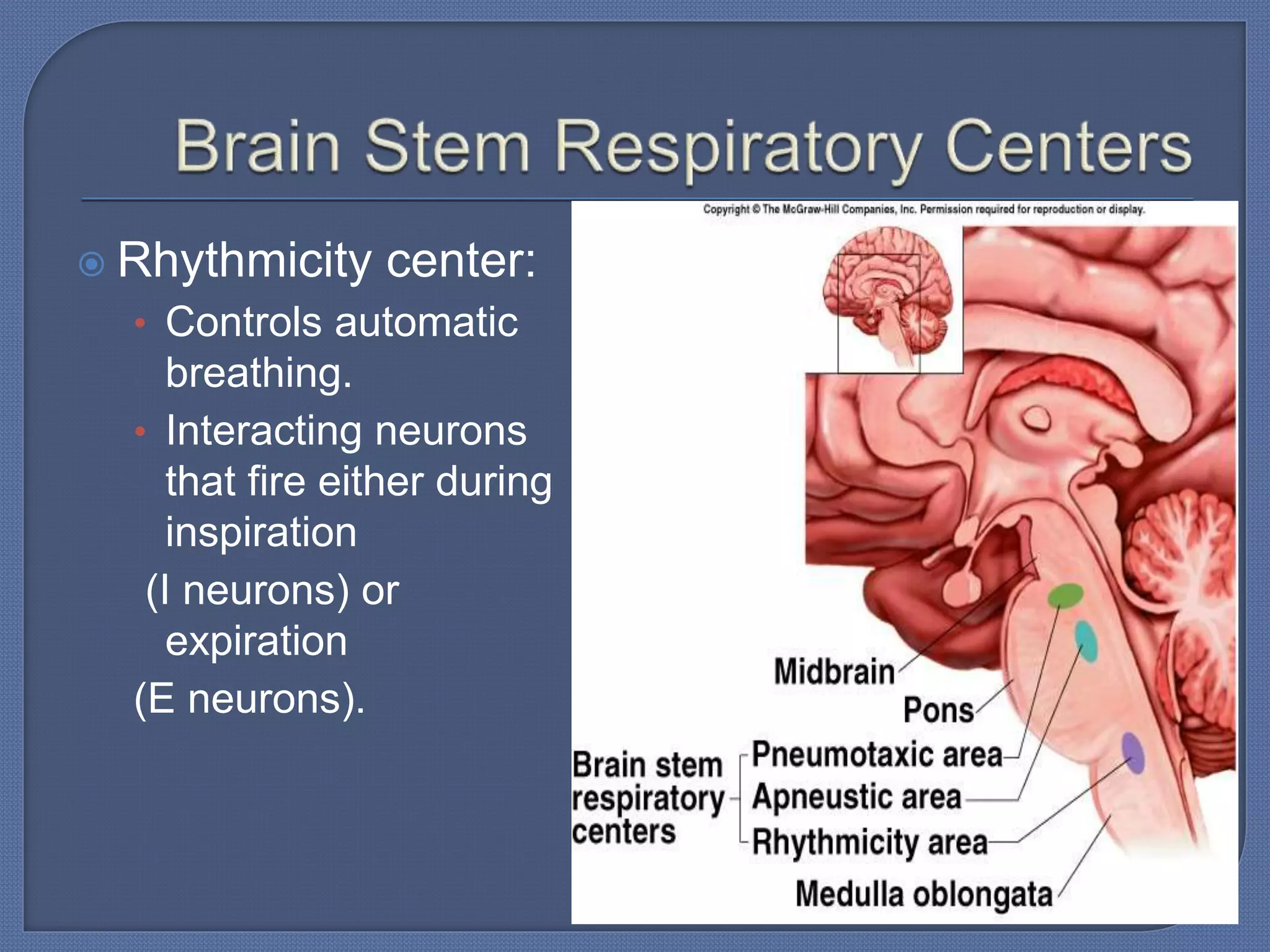
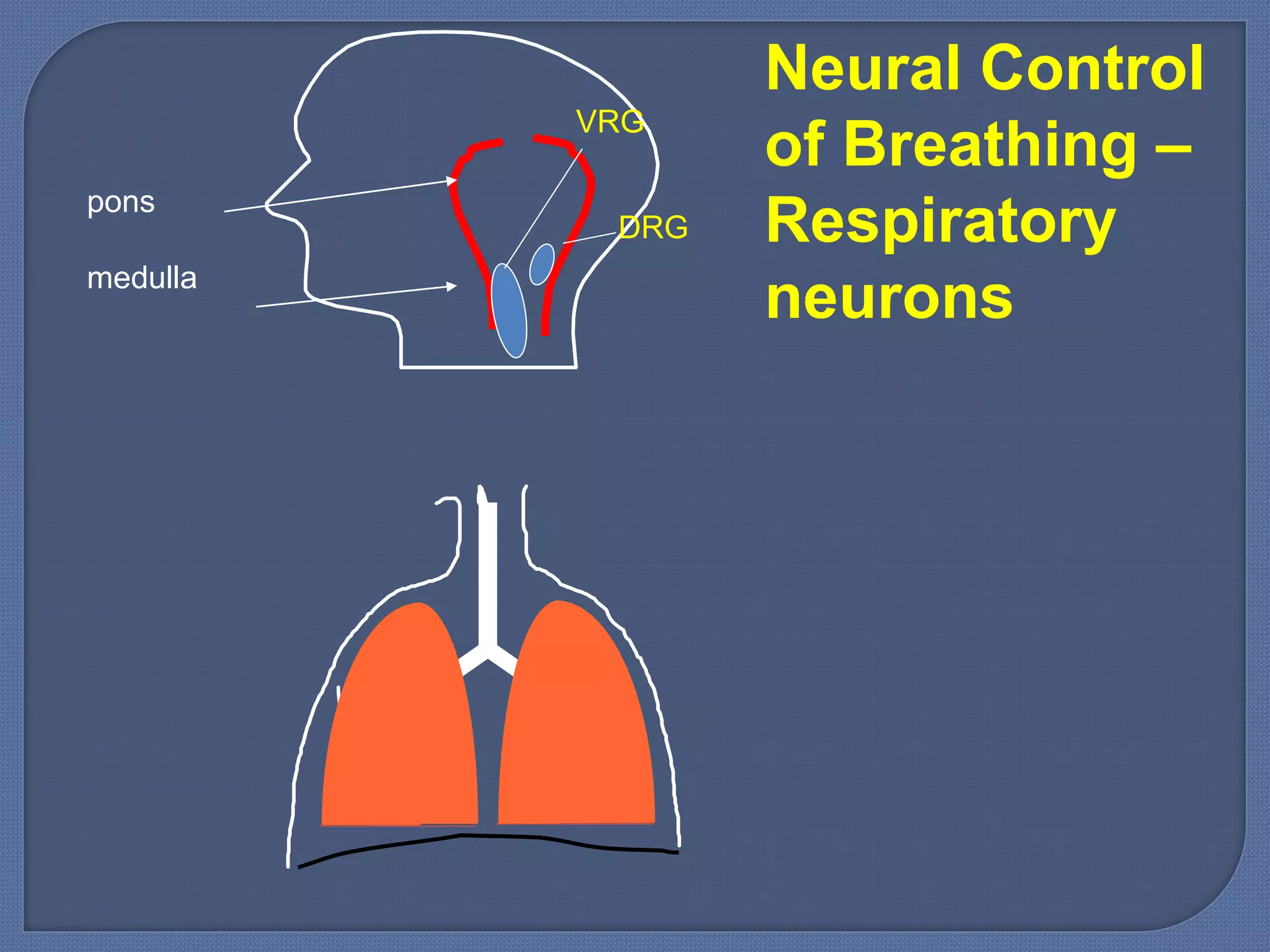
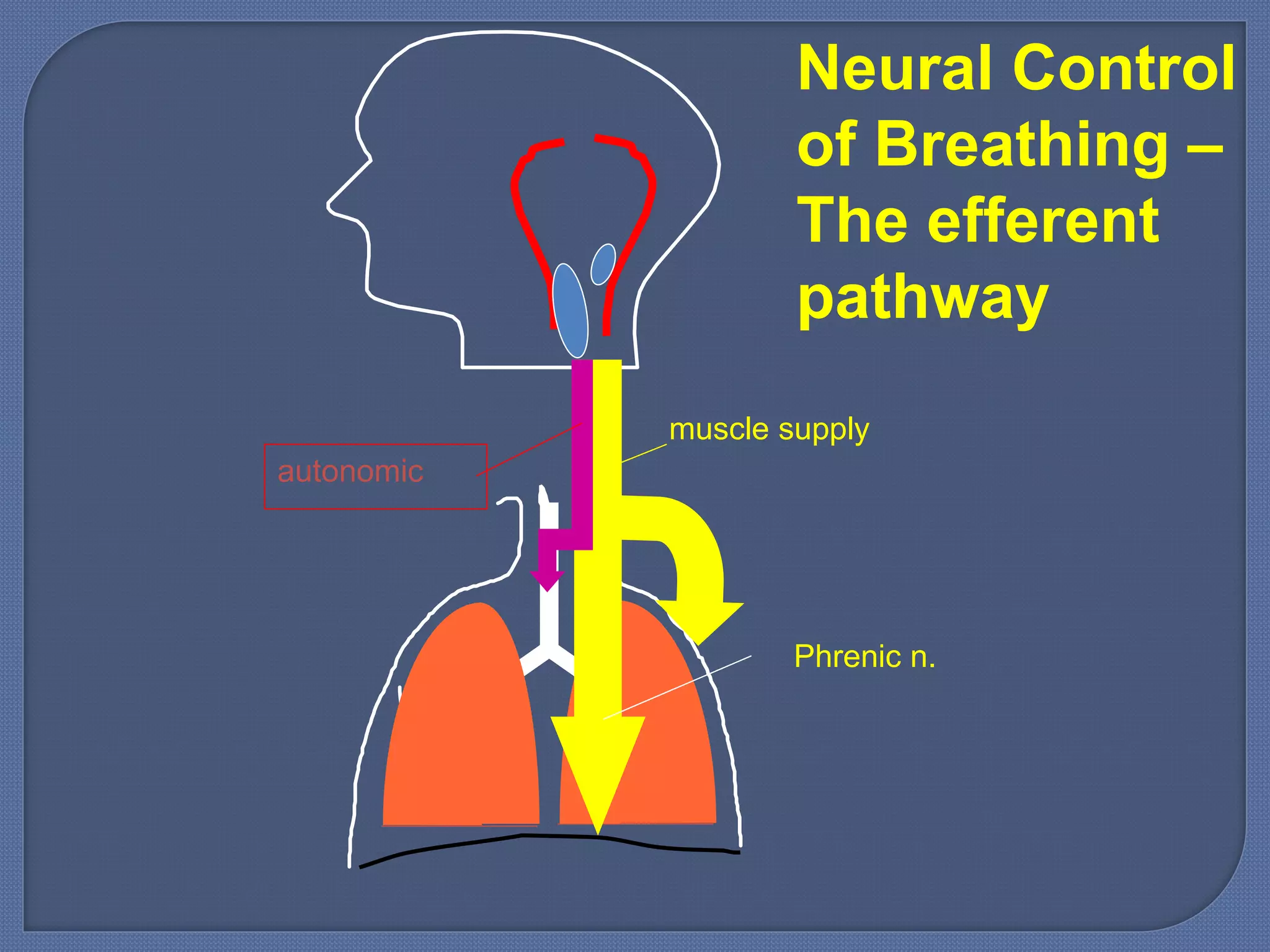
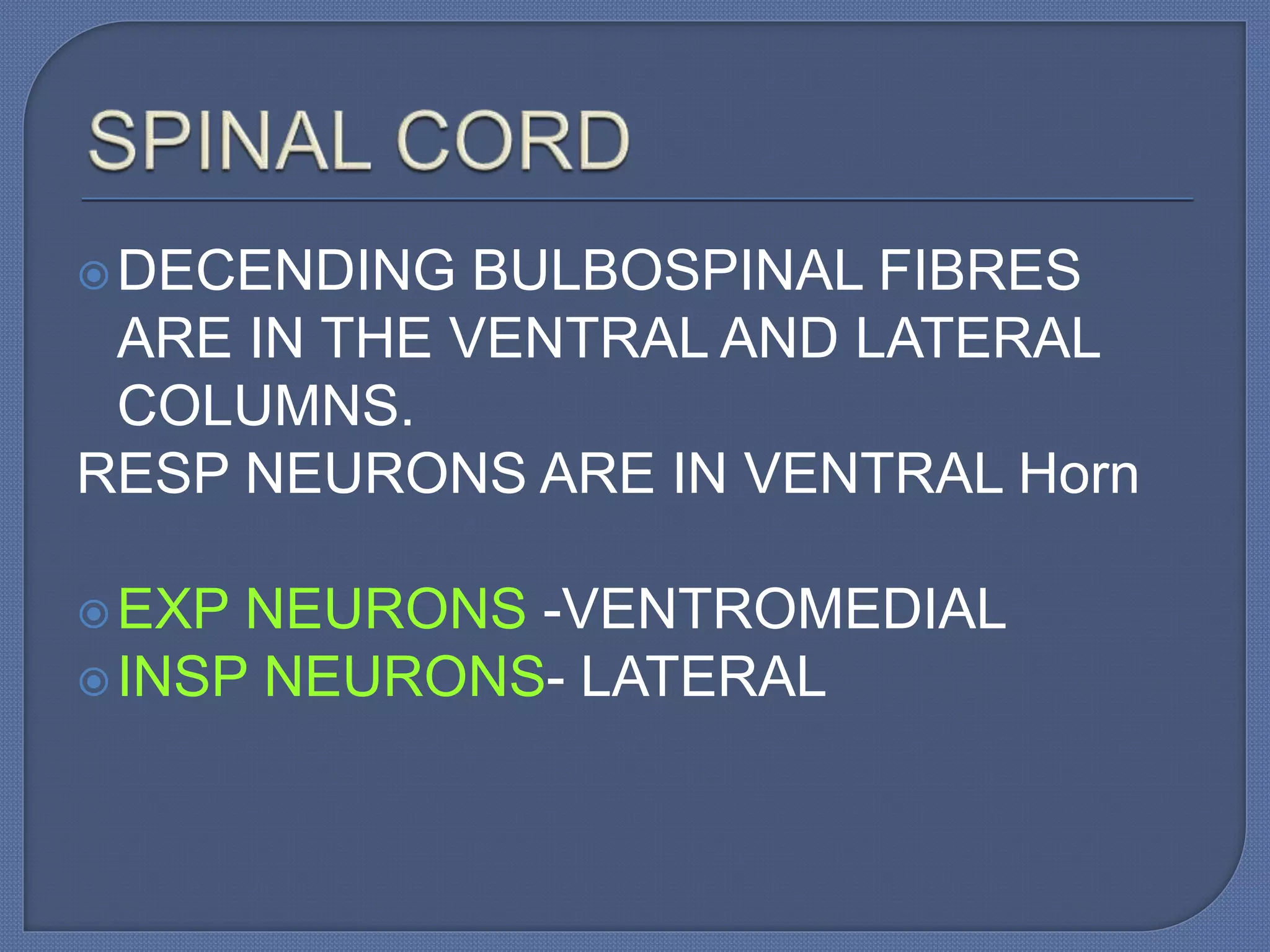
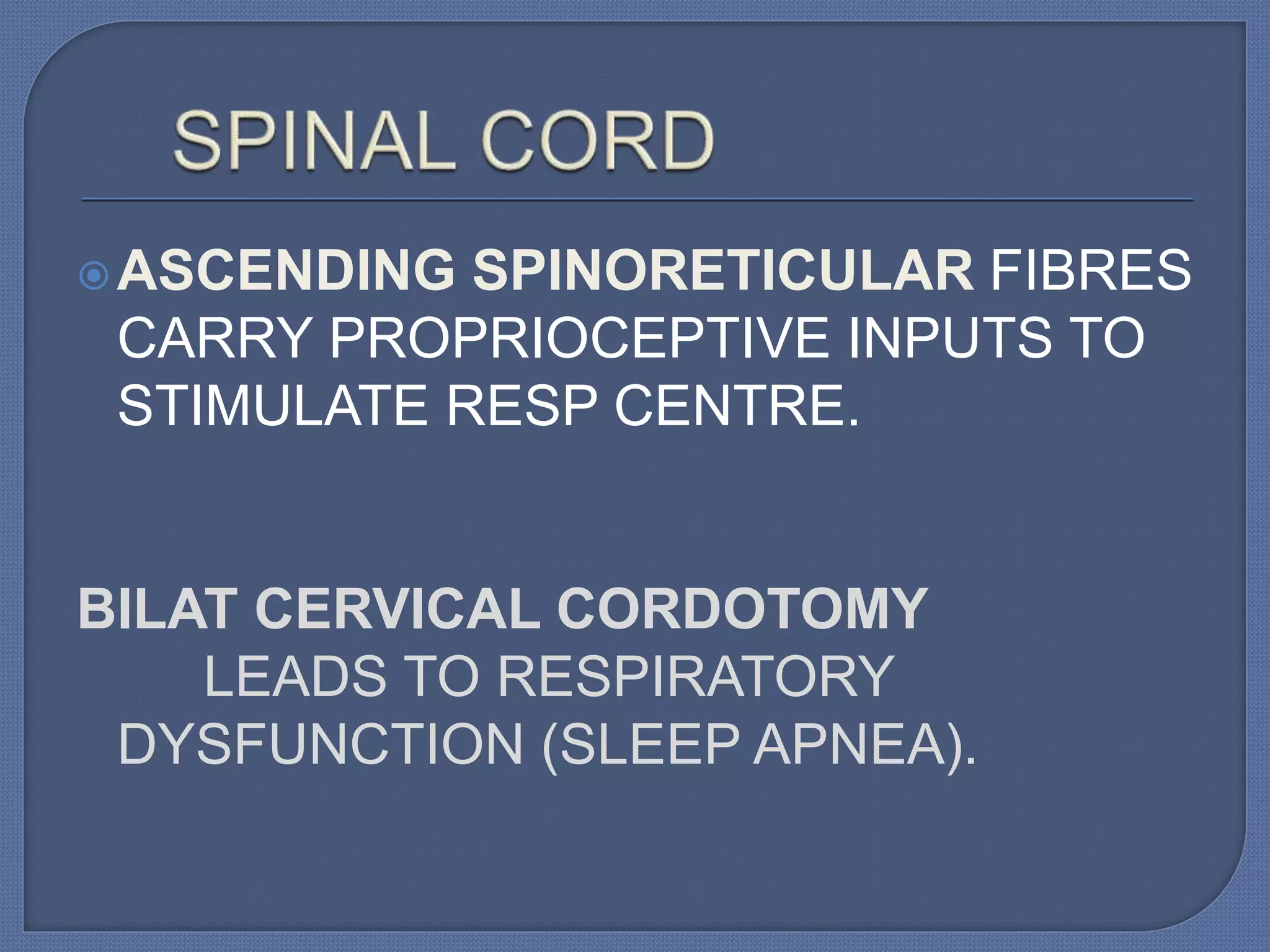
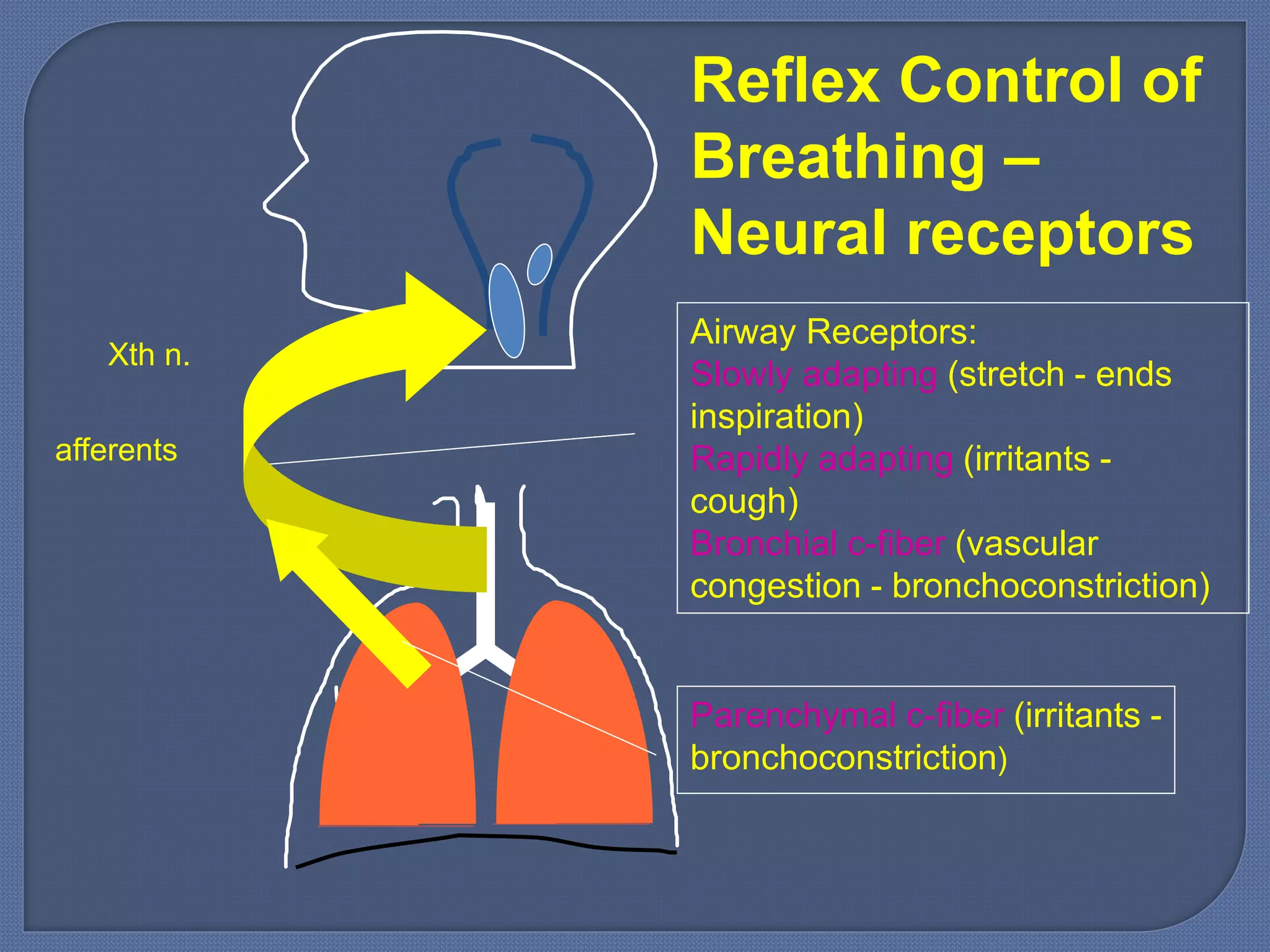
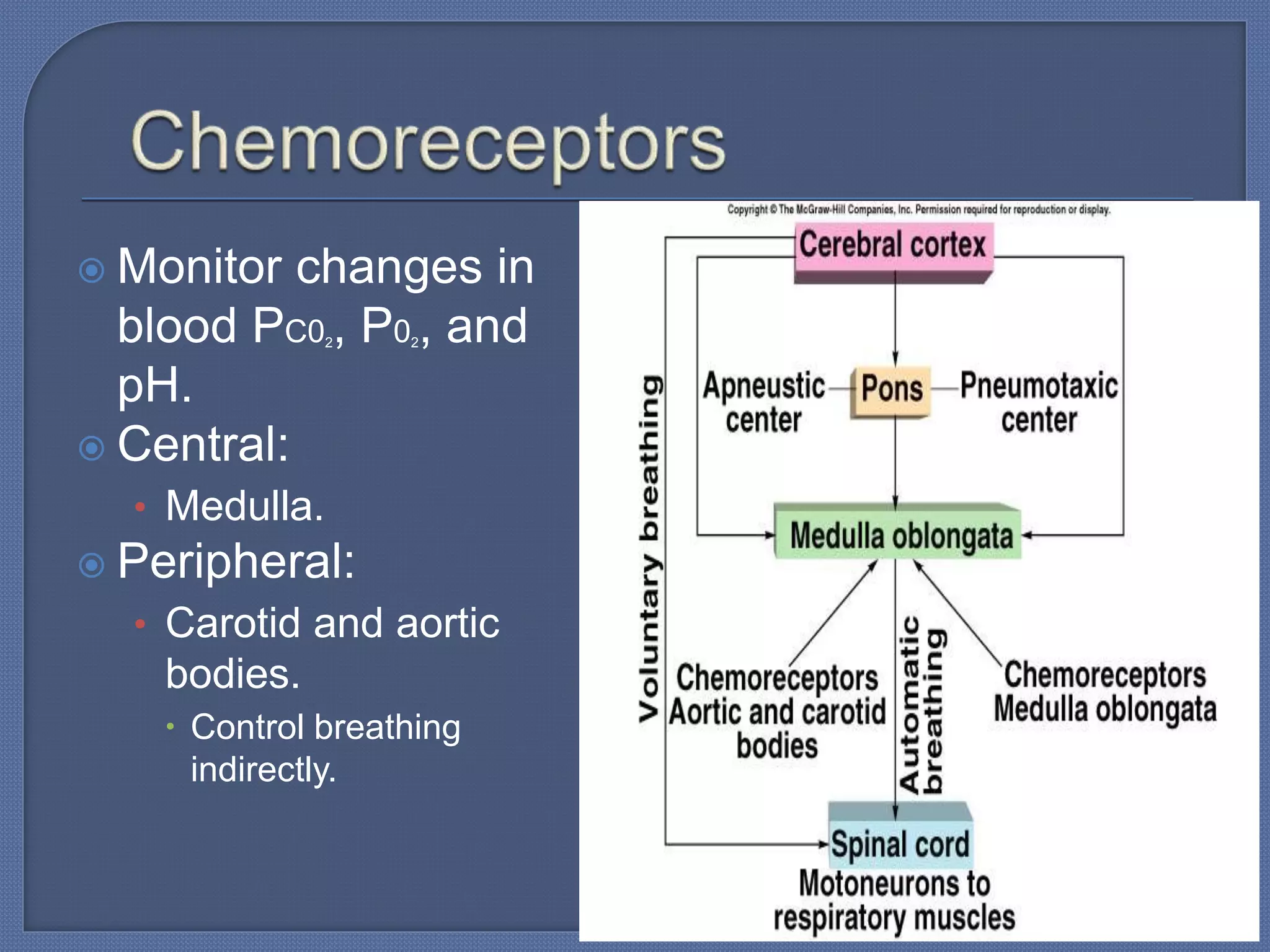
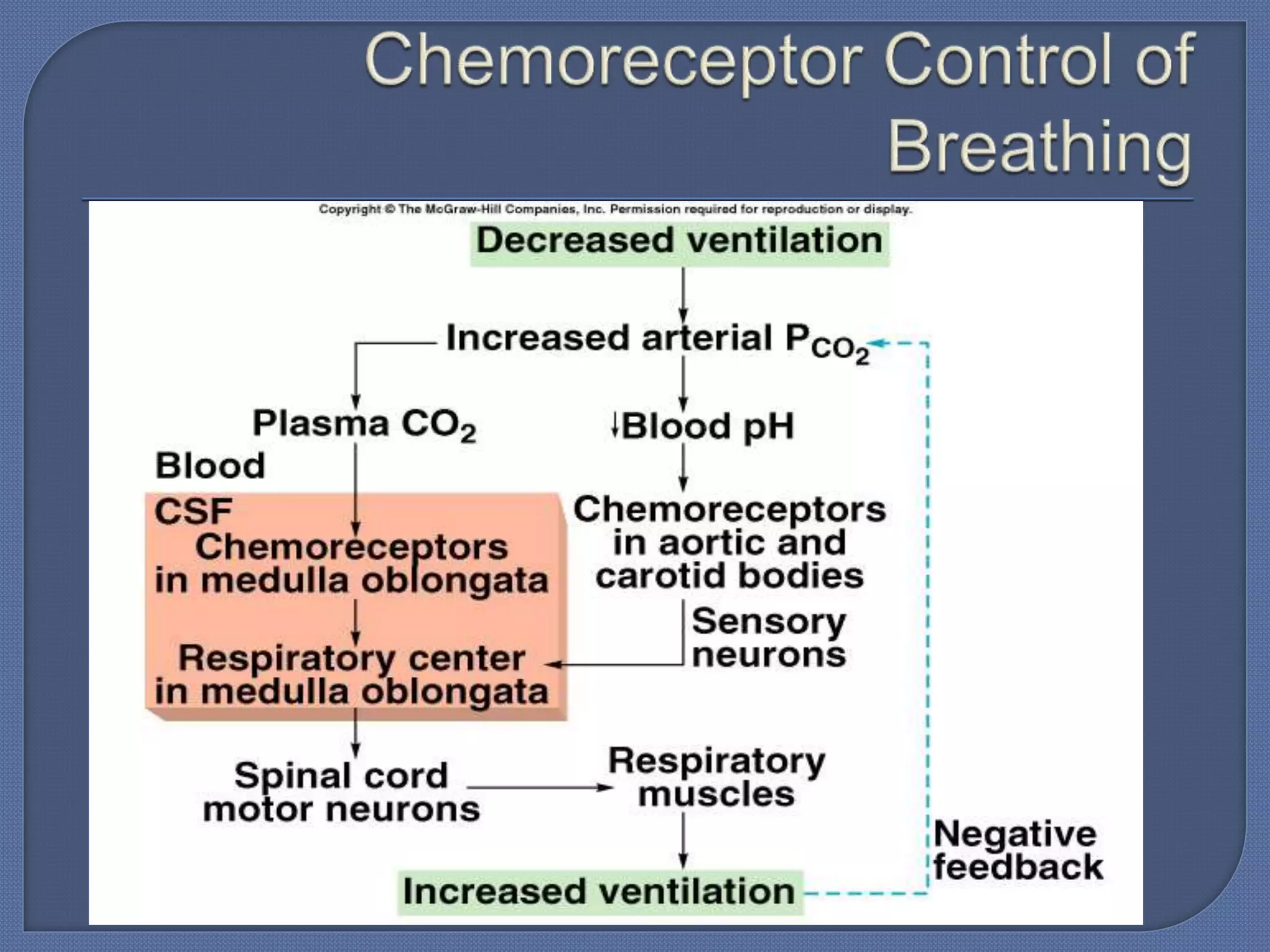
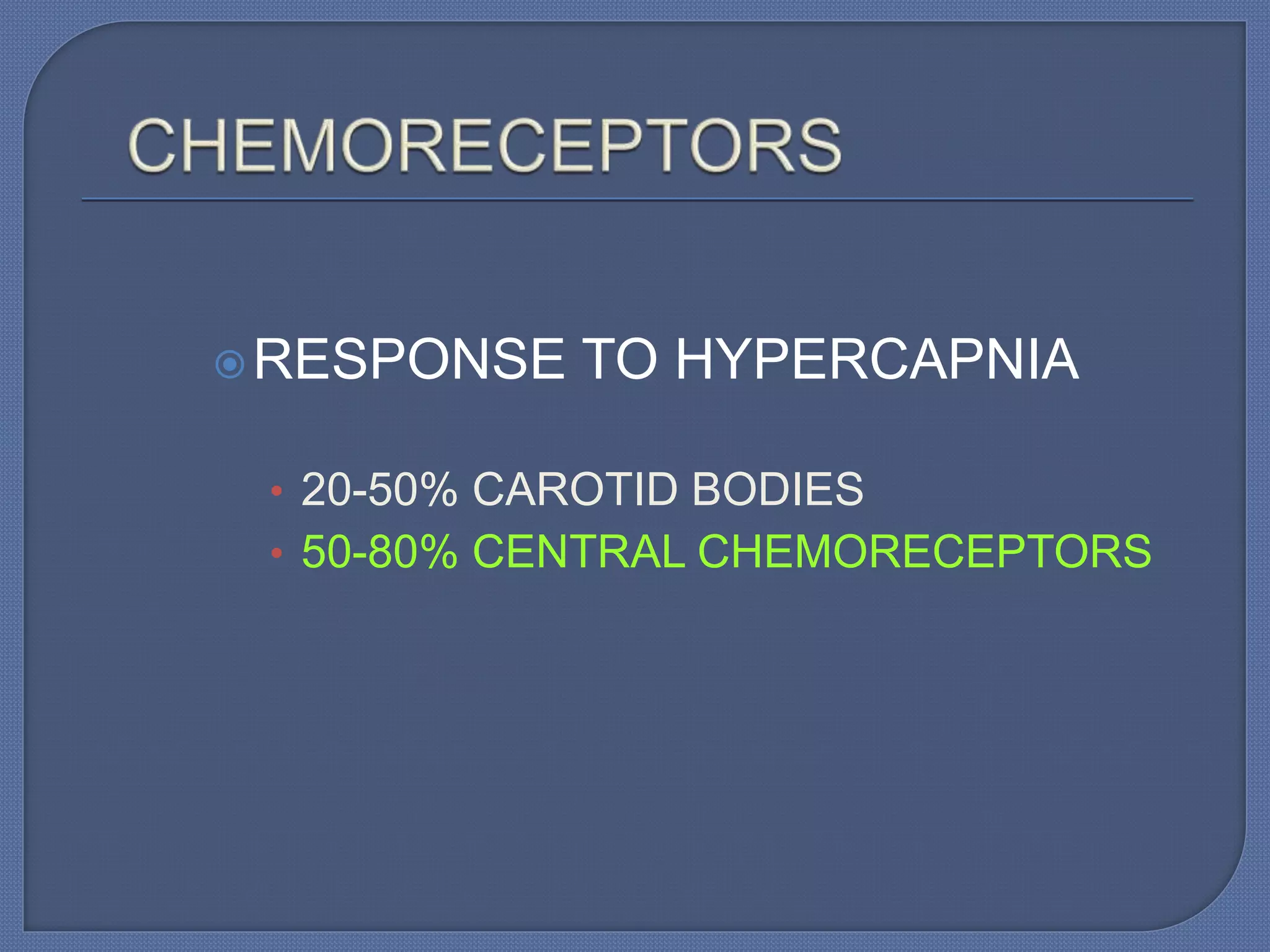
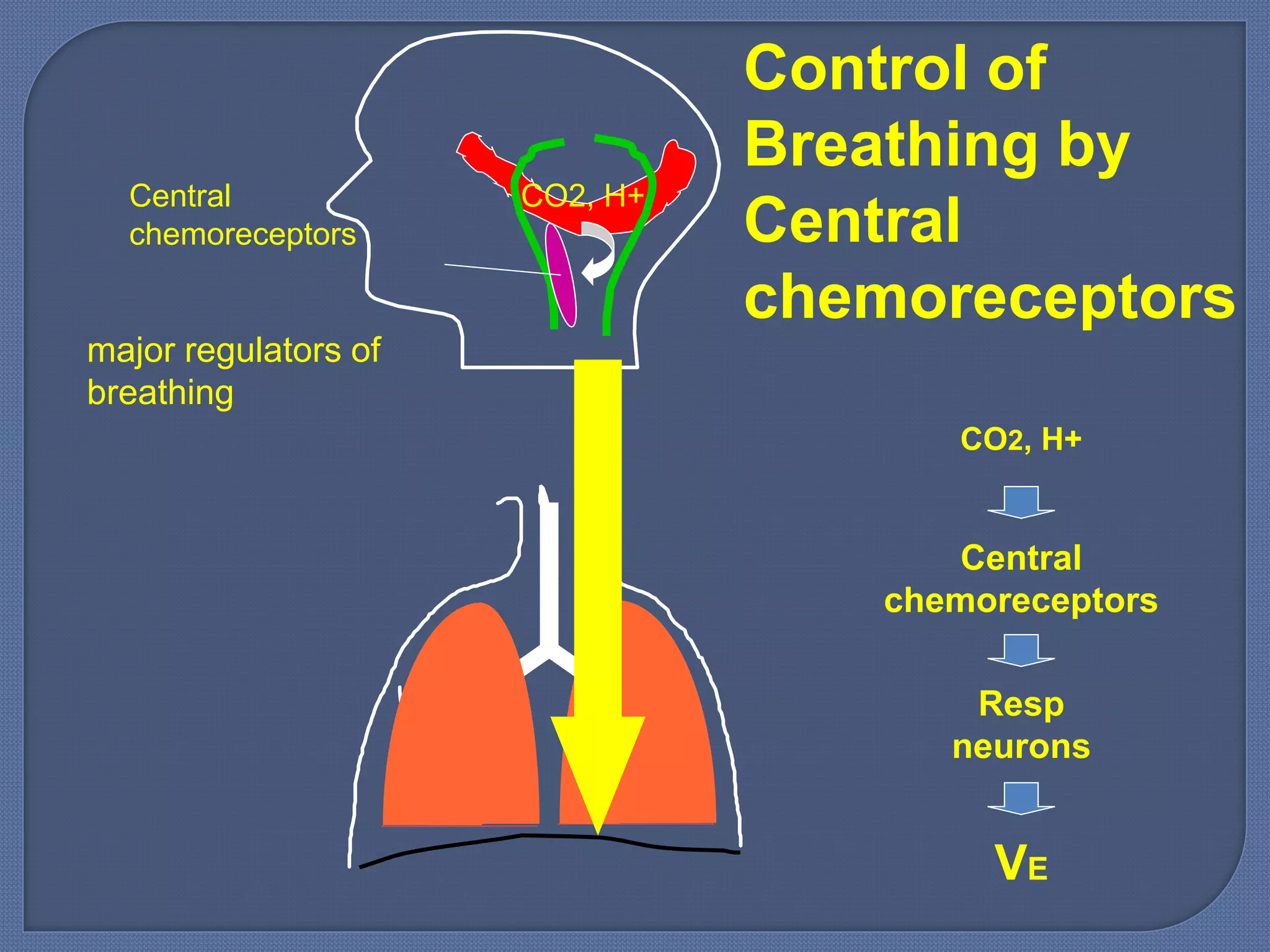
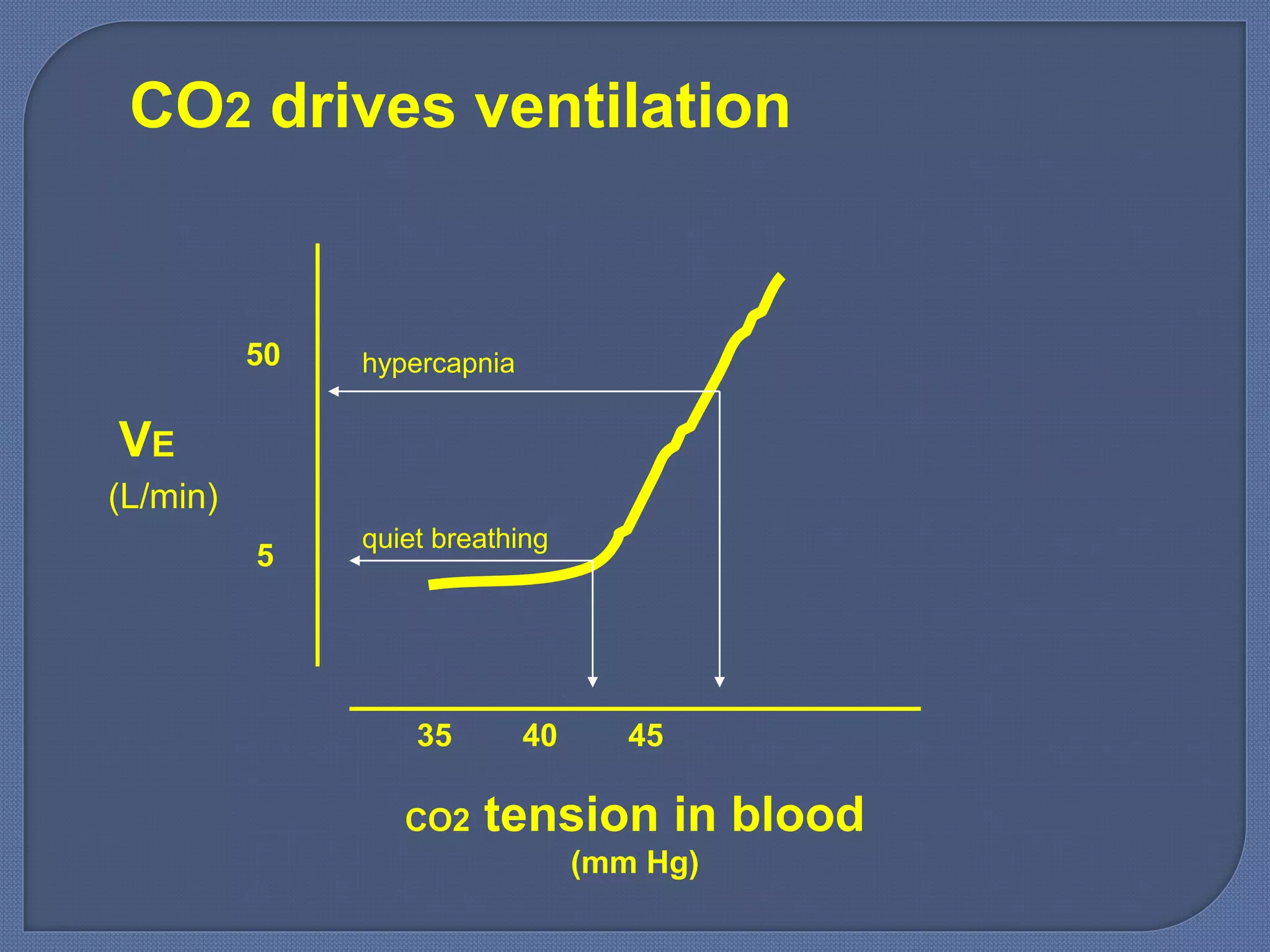
The document summarizes the neural control of breathing. It discusses how breathing is regulated by central neuronal networks in the brainstem and spinal cord to meet metabolic demands. The central neurons in the medulla and pons form the basic respiratory center that produces and controls respiration. These centers integrate input from higher brain areas, mechanoreceptors, and peripheral chemoreceptors. They regulate breathing frequency and tidal volume through motor neurons that control respiratory muscles. Chemical control of breathing also occurs through central and peripheral chemoreceptors that sense changes in blood gases like oxygen and carbon dioxide to modulate ventilation.
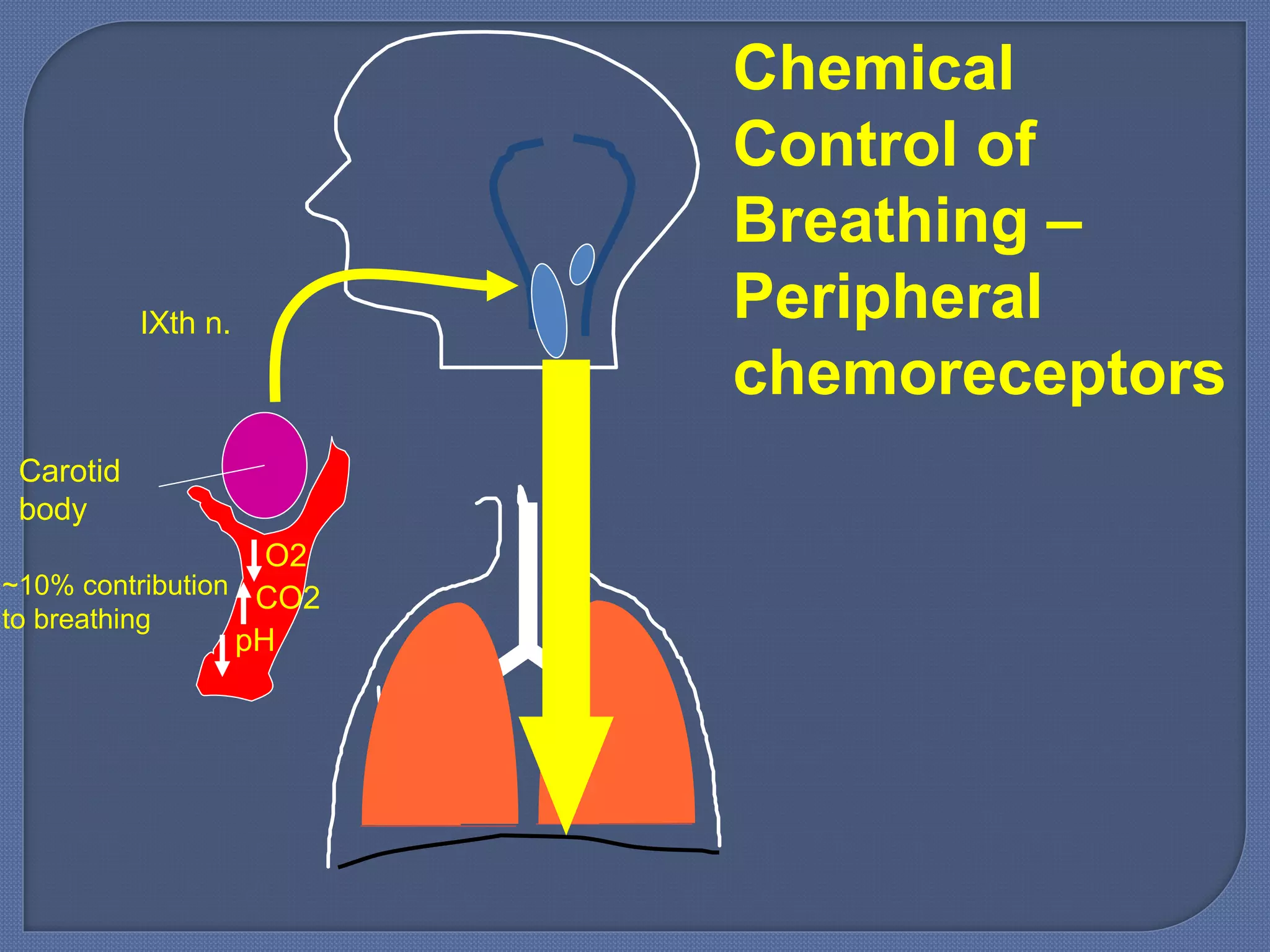
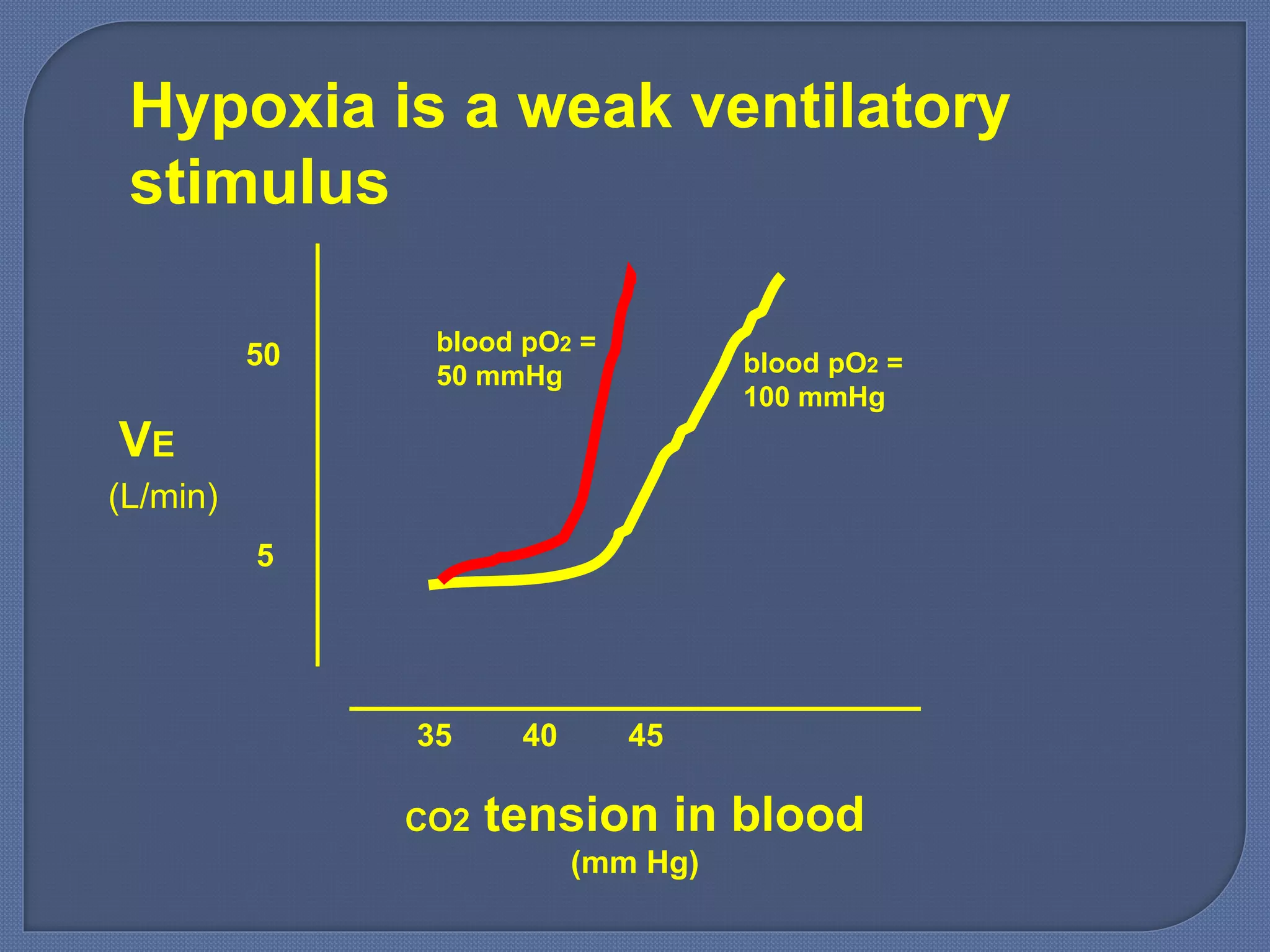
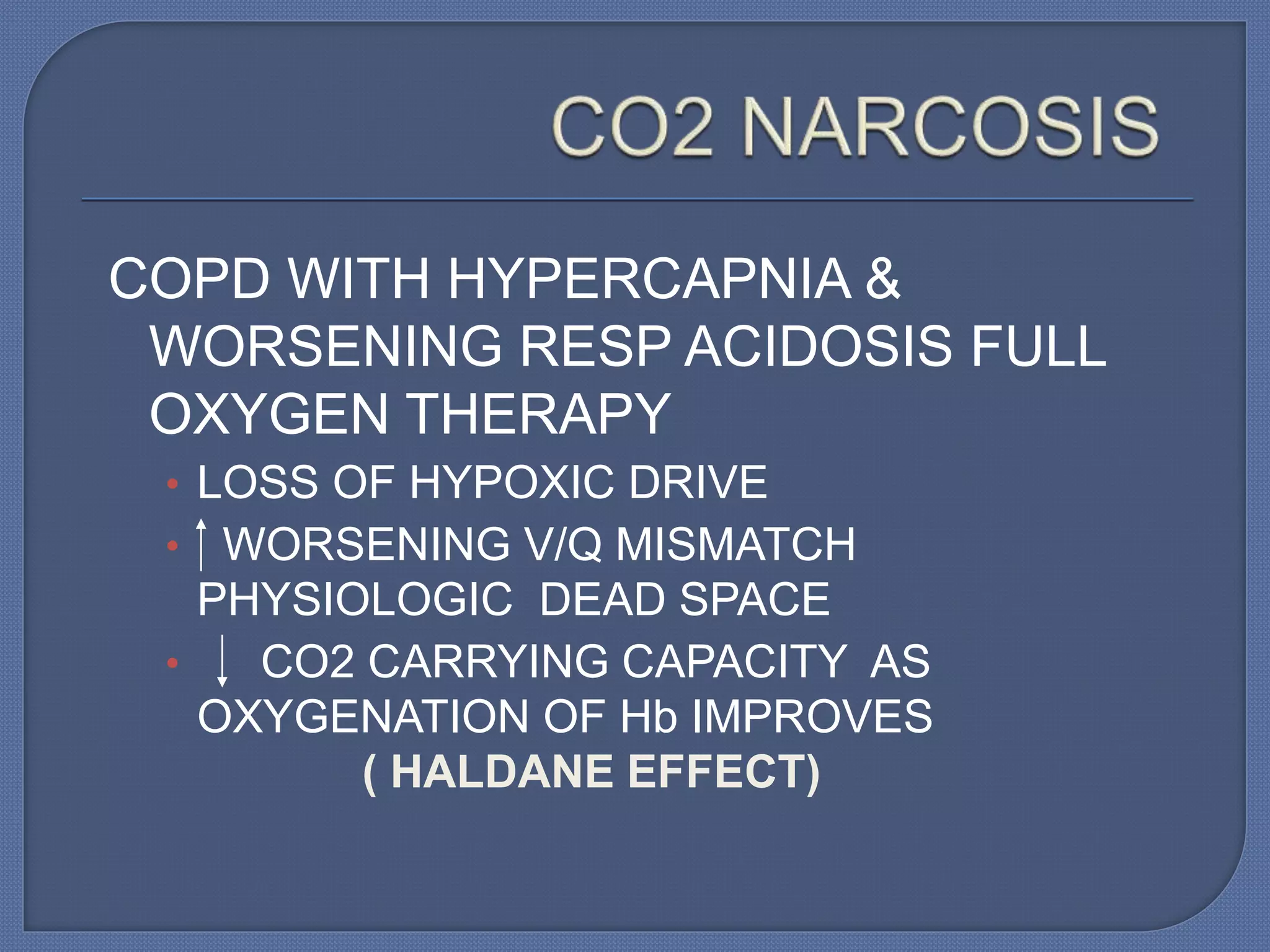
![Are not stimulated directly by changes in
arterial PC02.
H20 + C02 H2C03 H+
Stimulated by rise in [H+] of arterial blood.
• Increased [H+] stimulates peripheral
chemoreceptors.](https://image.slidesharecdn.com/control2-140611173254-phpapp01/75/Control-o-44-2048.jpg)