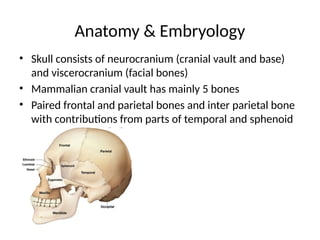
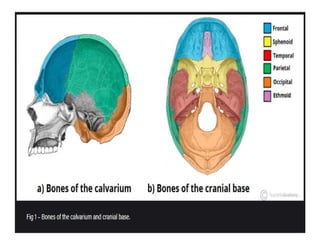
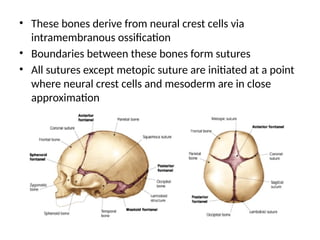
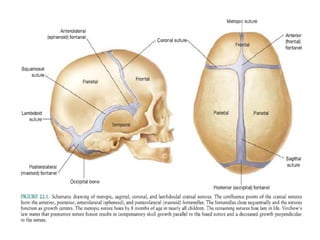
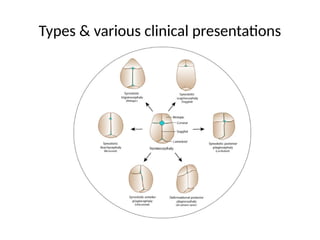
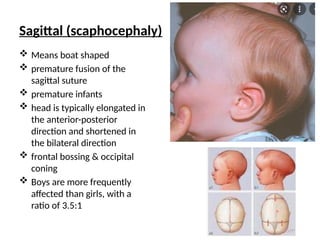
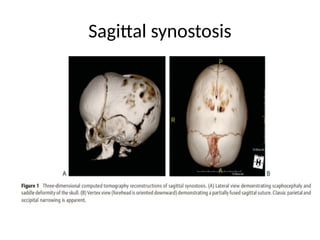
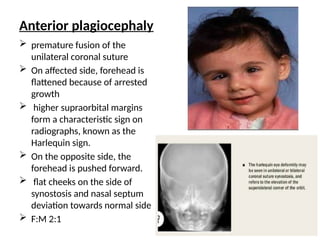
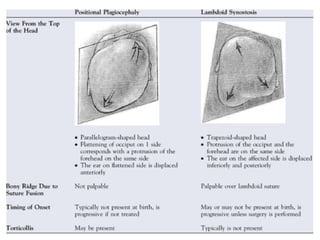
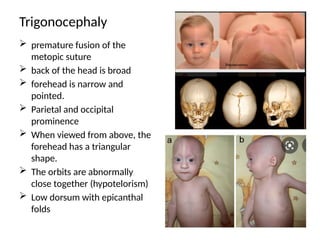
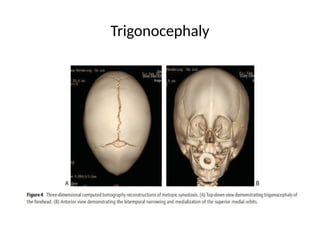
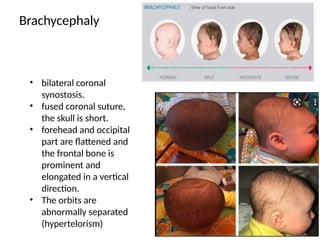
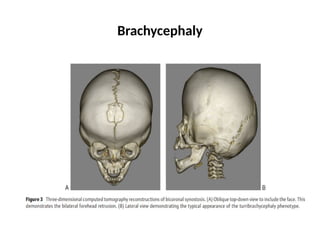
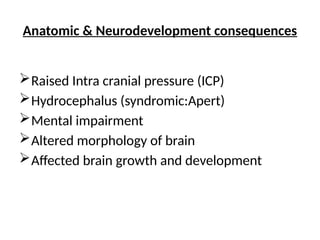
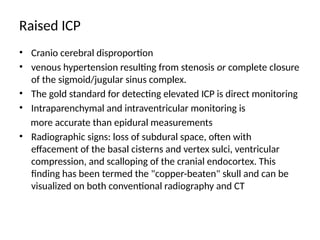
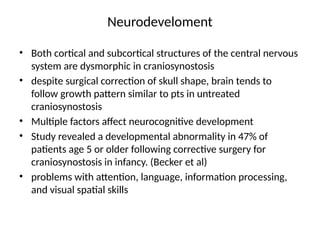
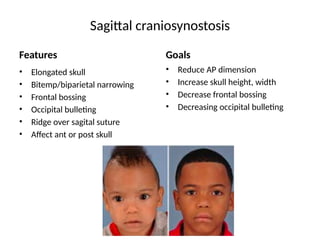
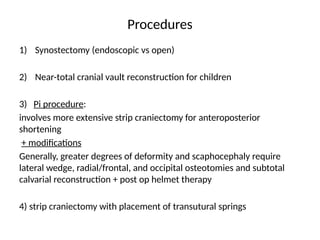
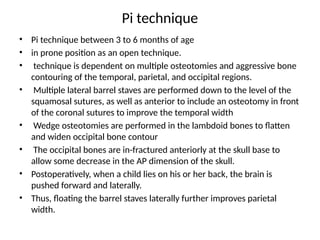
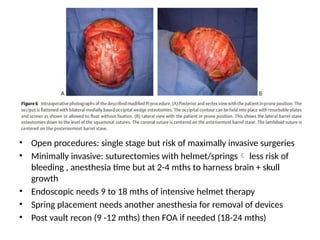
The document discusses nonsyndromic craniosynostosis, highlighting it as a condition characterized by premature fusion of cranial sutures leading to various craniofacial deformities and potential neurocognitive impairments. It reviews anatomy, epidemiology, pathogenesis including genetic factors, and clinical presentations, as well as details on surgical management and the implications of timing in intervention. Emphasis is placed on the importance of early diagnosis and comprehensive treatment approaches for positive outcomes.