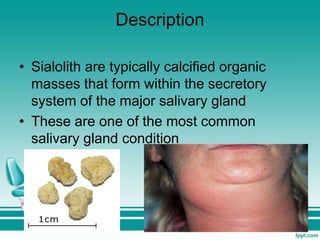
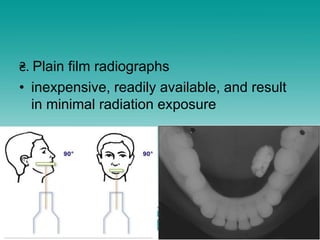
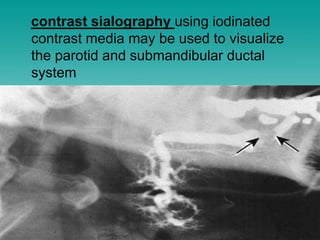
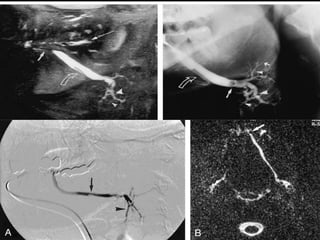
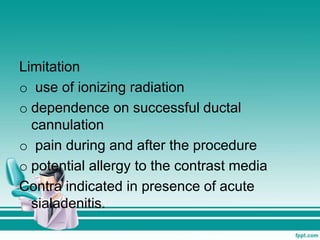
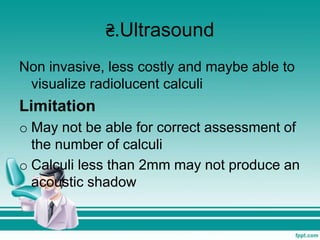
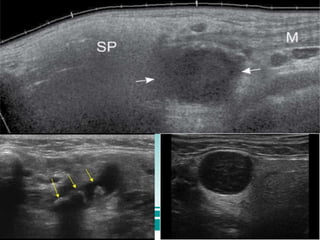
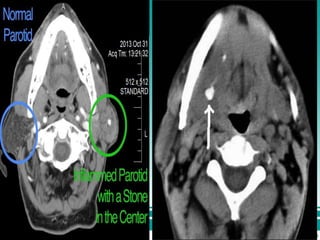
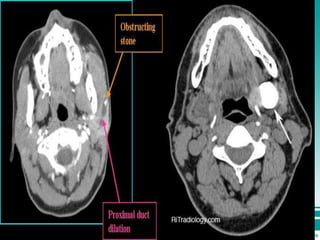
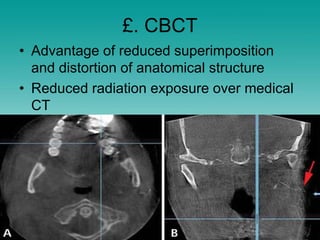
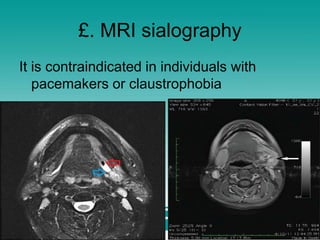
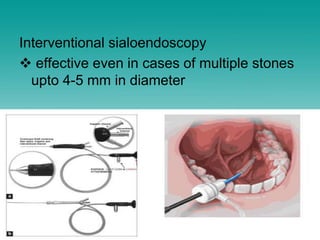
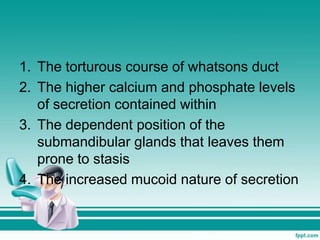
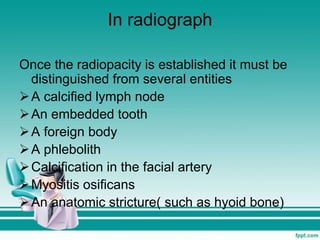
Sialolithiasis is the formation of calcified masses within salivary glands, primarily affecting the submandibular gland. The condition is associated with factors that promote saliva retention and alterations in saliva composition, leading to symptoms such as pain, swelling, and potential complications like infection or gland atrophy. Diagnosis may involve imaging techniques such as radiographs and CT scans, while treatment can include supportive care, sialoendoscopy, or surgical options in advanced cases.