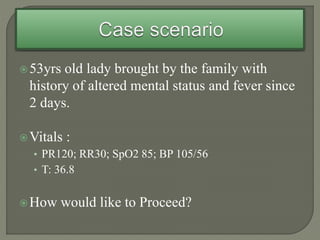
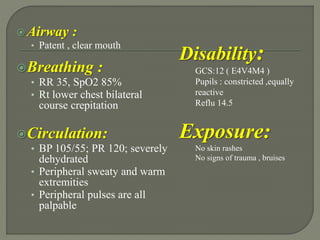
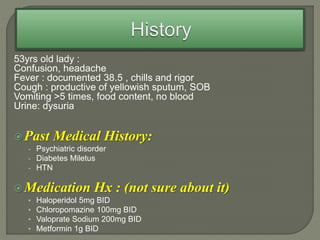
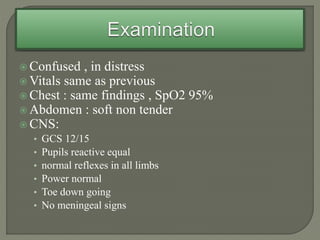
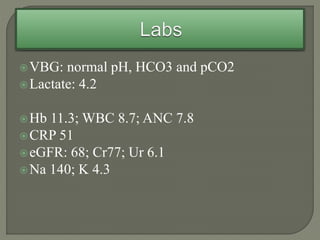
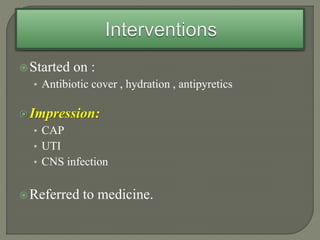
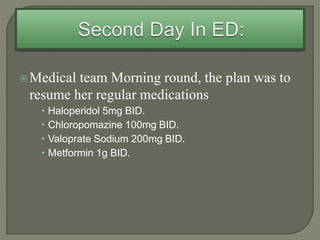
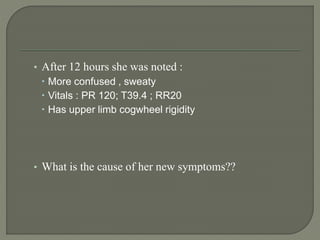
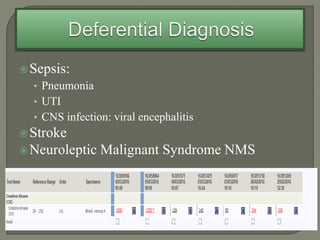
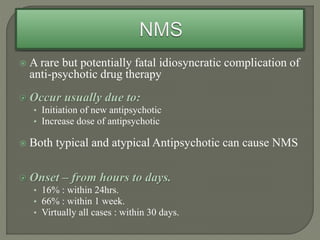
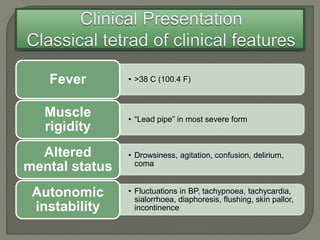
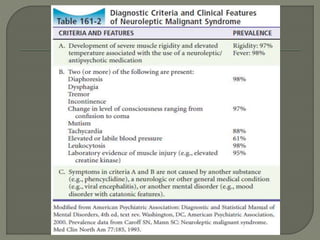
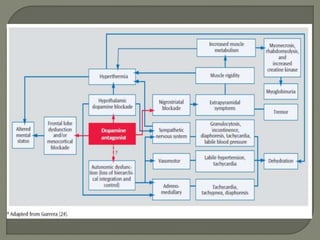
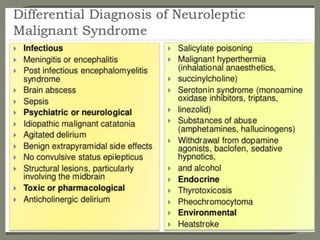
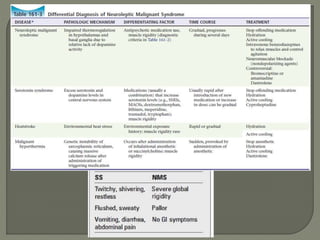
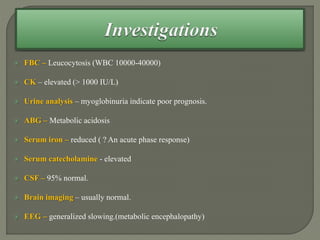
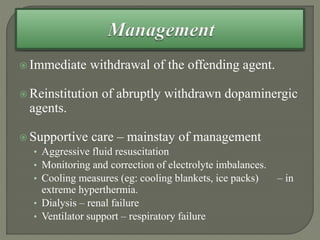
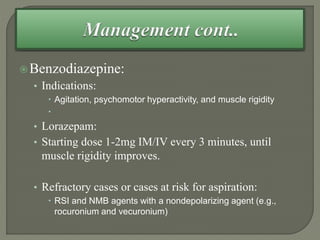
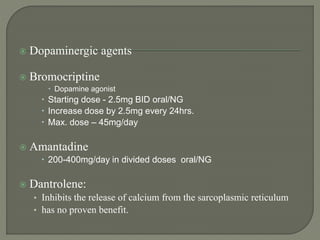
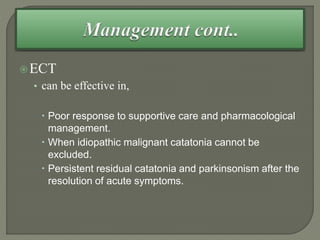
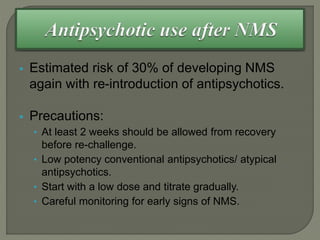
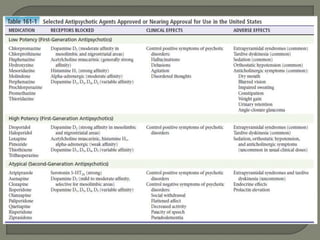
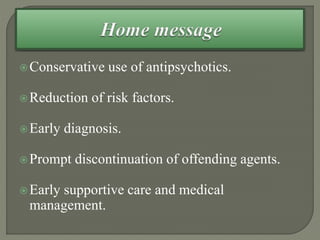
This document describes the case of a 53-year-old lady brought in with altered mental status and fever. Her symptoms worsened after 12 hours, with increased confusion and rigidity. This was likely caused by neuroleptic malignant syndrome (NMS), a rare but serious reaction to antipsychotic drugs. NMS requires immediate withdrawal of antipsychotics, supportive care, and may include benzodiazepines or dopaminergic drugs. Careful monitoring is needed if antipsychotics are reintroduced.