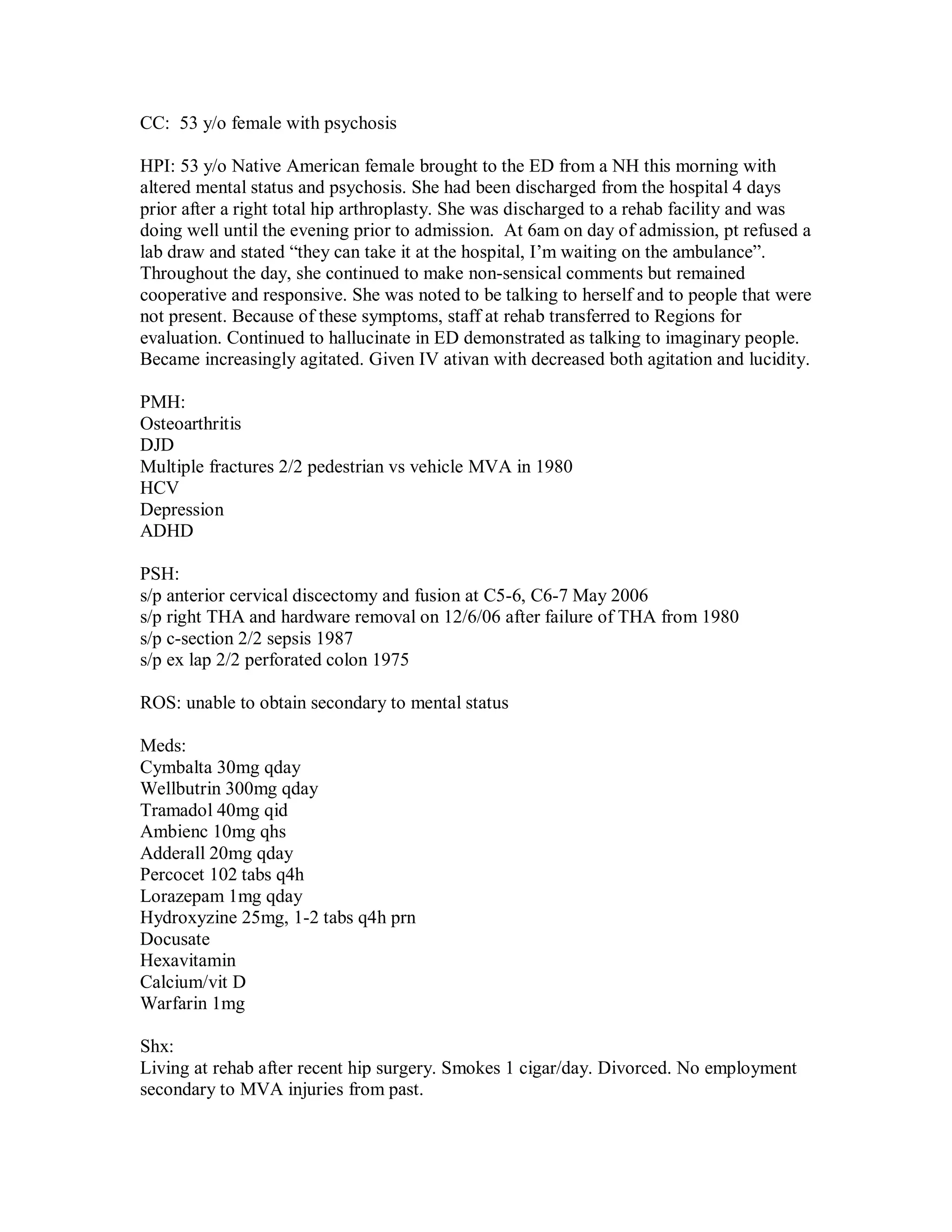
1) 53 year old Native American female with history of osteoarthritis, depression, ADHD presented with altered mental status and psychosis 4 days after hip surgery.
2) On examination, she was agitated and diaphoretic with tremors in lower extremities and hyperreflexia. Labs showed elevated CK consistent with serotonin syndrome.
3) She was diagnosed with likely serotonin syndrome from an interaction between her antidepressants and possible amphetamine or THC use, and was admitted to the ICU.