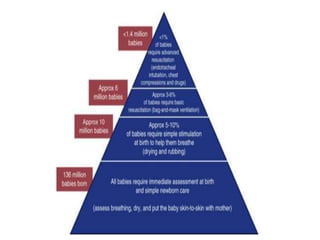
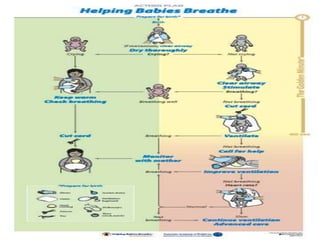
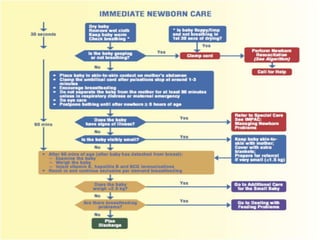
This document discusses guidelines for resuscitating newborn babies. It describes how the placenta is clamped off at birth, requiring the newborn to breathe on their own. The Helping Babies Breathe (HBB) program teaches techniques to evaluate the airway, establish breathing and circulation for babies. It outlines initial steps like drying the baby thoroughly and putting them skin-to-skin with the mother. If the baby does not start breathing on their own after 30 seconds of drying, providers should reposition, suction and provide ventilation if needed. The full resuscitation protocol, including ventilation, chest compressions and medications like epinephrine, is described to help newborns transition successfully after birth.