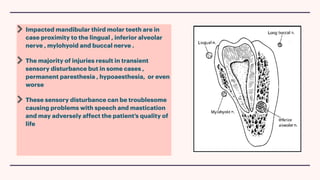
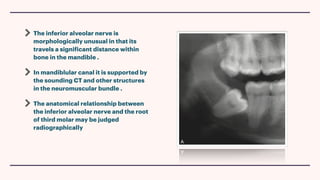
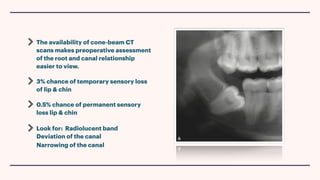
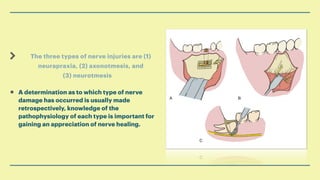
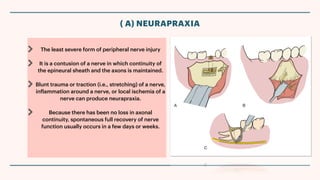
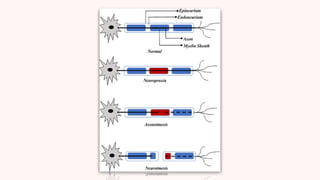
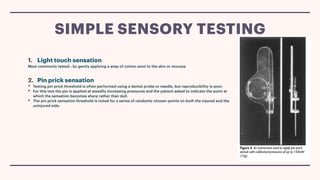
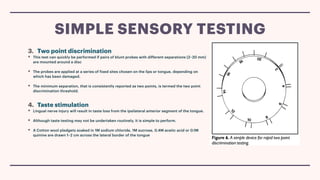
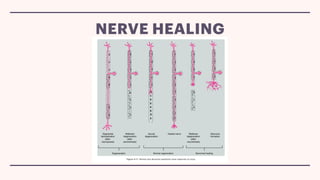
This document discusses nerve injuries that can occur during third molar extraction, including injuries to the inferior alveolar nerve and lingual nerve. It describes the classification of nerve injuries into neurapraxia, axonotmesis, and neurotmesis based on the severity of damage. Methods for monitoring nerve recovery include light touch, pin prick, and two-point discrimination testing. Nerve healing occurs through degeneration and regeneration phases, with Wallerian degeneration occurring after severe nerve trauma. Proper management of nerve injuries includes diagnosis, monitoring recovery, and treatment if needed.