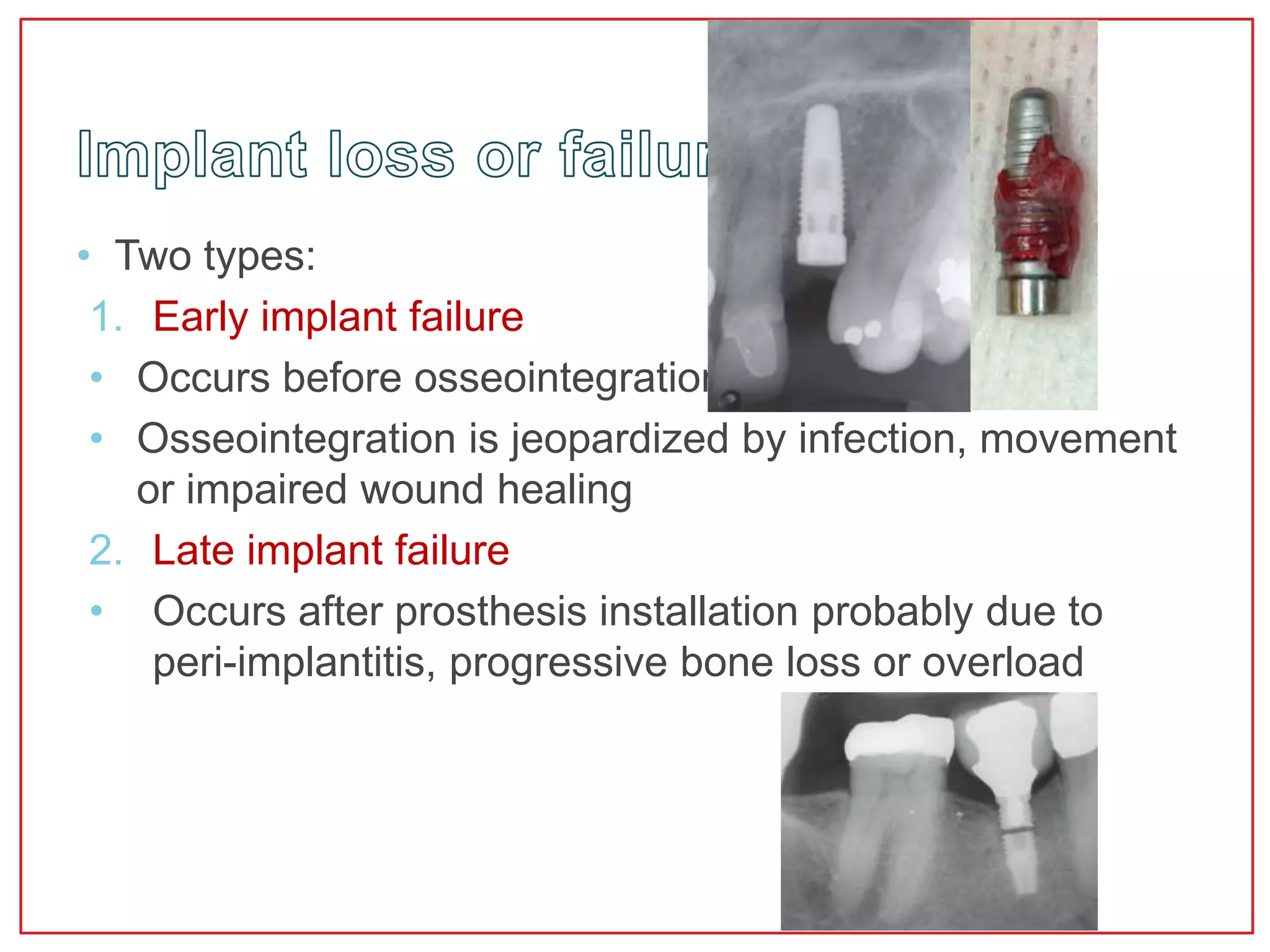
This document discusses complications related to dental implants. It begins by discussing surgical complications such as hemorrhage, hematoma, neurosensory disturbances, and implant malposition. It then discusses biological complications affecting the peri-implant soft tissues, such as inflammation, recession, and progressive bone loss which can lead to peri-implantitis. Mechanical complications are also summarized, including screw loosening/fracture and implant fracture.