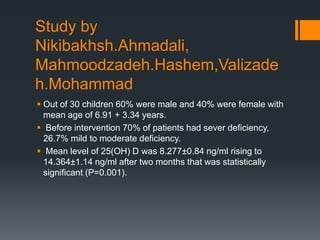
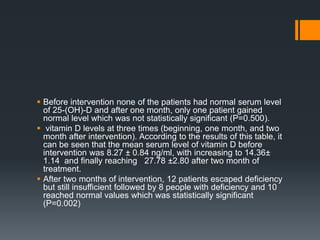
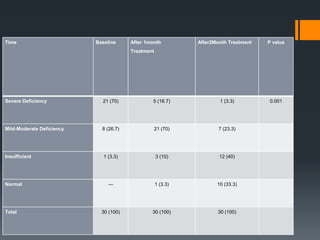
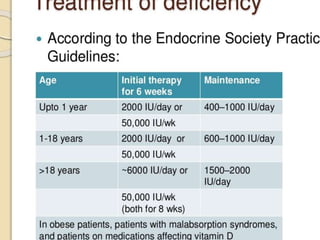
The document discusses the implications of vitamin D deficiency in children with nephrotic syndrome, highlighting its multi-factorial causes and systemic effects such as hypocalcemia and cardiovascular disease. It notes that while vitamin D levels improve significantly with supplementation during treatment, full normalization is rare, suggesting a need for routine monitoring and individualized approaches for management. Additionally, it covers the importance of combining vitamin D with other nutrients to mitigate potential bone loss from steroid therapy and the role of various vitamins in regulating health outcomes in these patients.