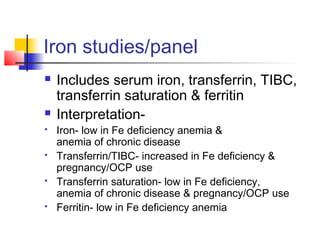
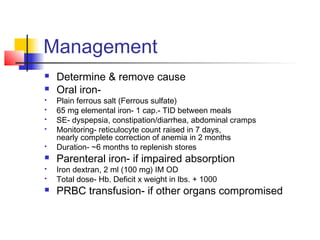
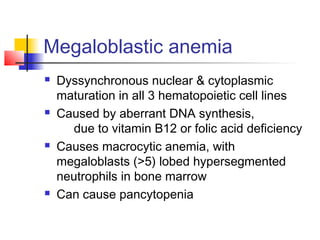
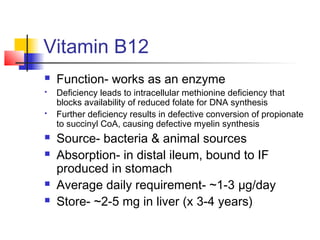
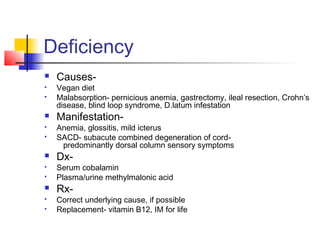
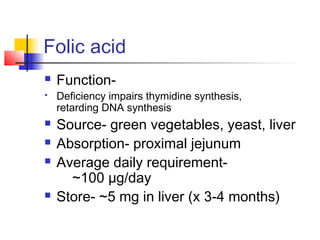
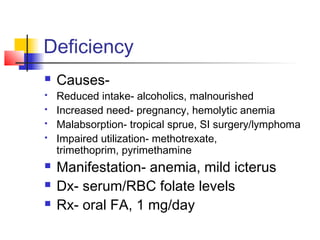
This document discusses nutritional anemias, including iron deficiency anemia and megaloblastic anemia caused by vitamin B12 or folic acid deficiency. It covers the metabolism and absorption of iron and these vitamins, causes of deficiency including diet and malabsorption, clinical manifestations of deficiency anemias, diagnostic tests, and management approaches including oral and parental supplementation.