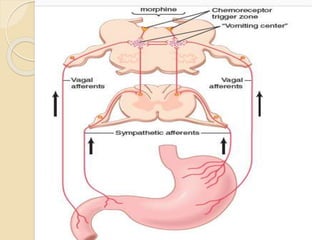
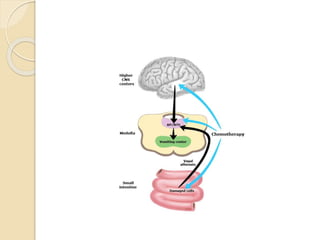
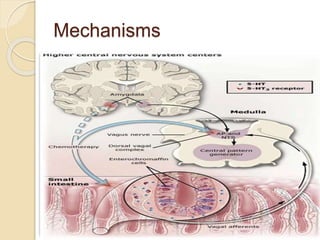
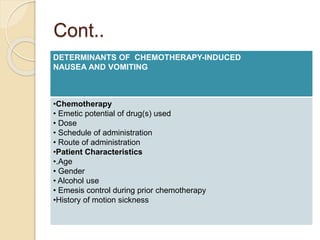
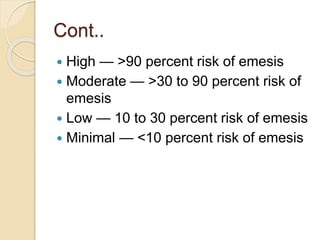
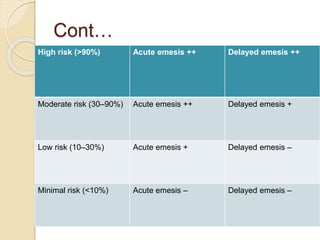
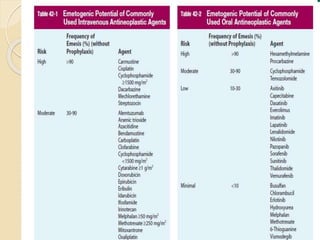
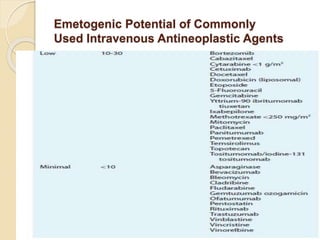
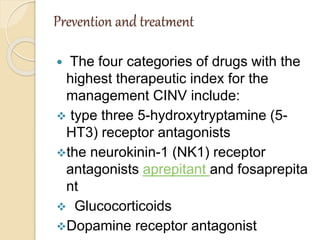
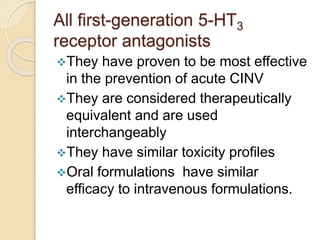
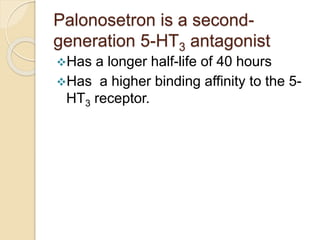
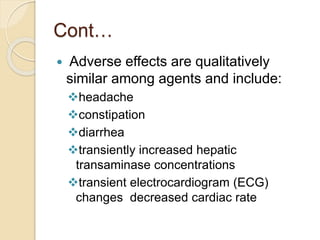
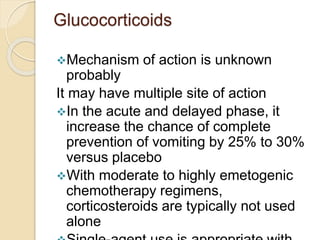
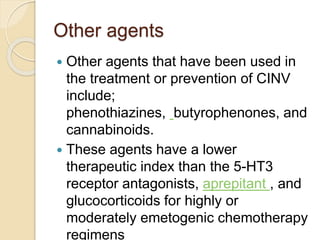
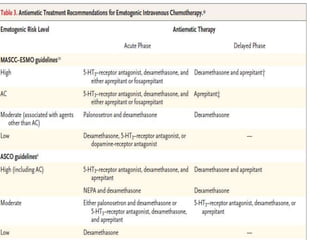
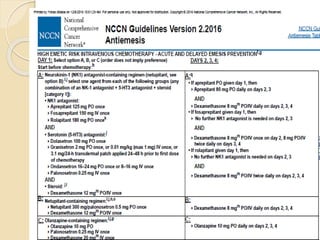
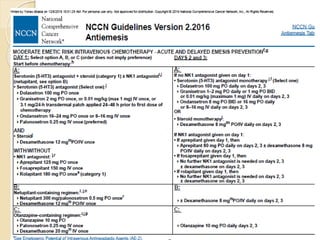
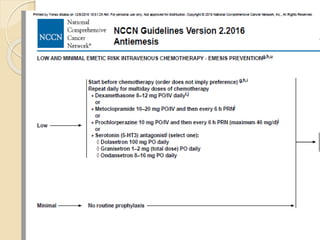
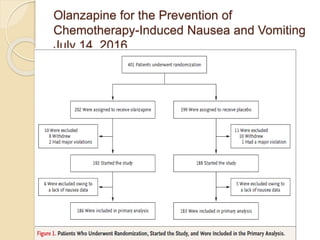
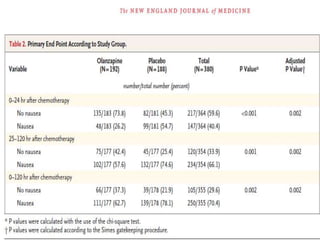
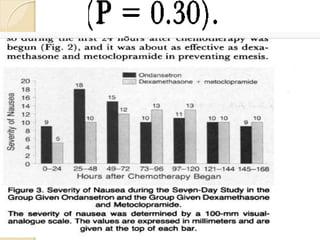
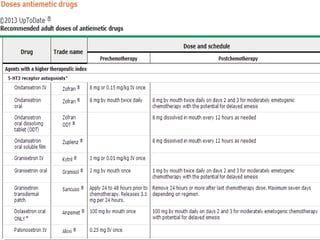
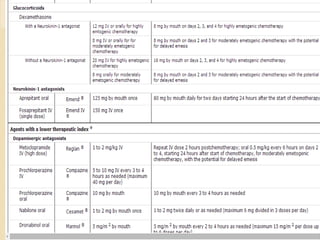
This document outlines chemotherapy-induced nausea and vomiting (CINV), including its types, pathophysiology, predictive factors, and prevention/treatment approaches. There are three types of CINV - acute, delayed, and anticipatory. The pathophysiology involves the central nervous system and neurotransmitters like dopamine, serotonin, and substance P. Predictive factors include the chemotherapy agent/dose, patient characteristics, and antiemetic regimen. Prevention/treatment involves 5-HT3 receptor antagonists, neurokinin-1 receptor antagonists, glucocorticoids, and dopamine receptor antagonists. Combination therapy is most effective at preventing both acute and delayed CINV.