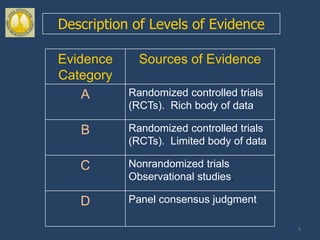
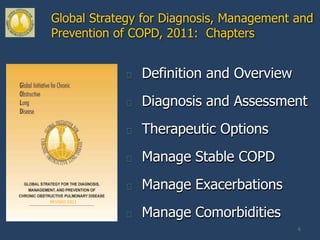
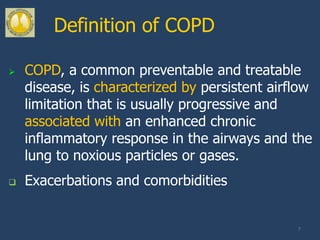
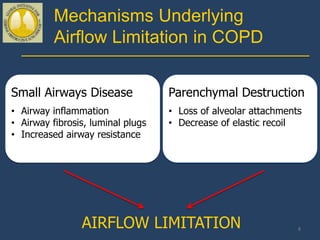
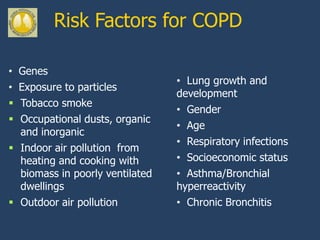
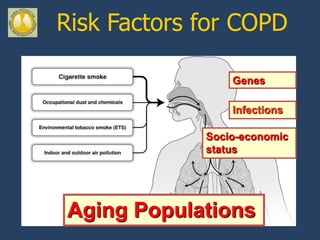
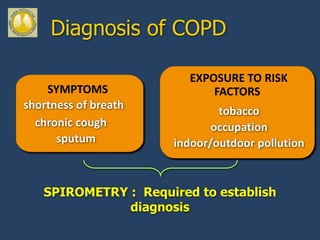
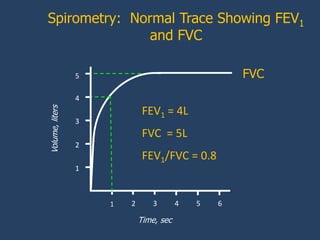
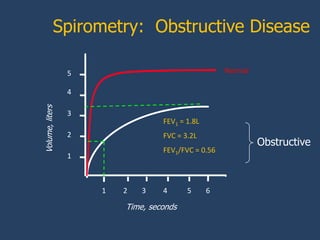
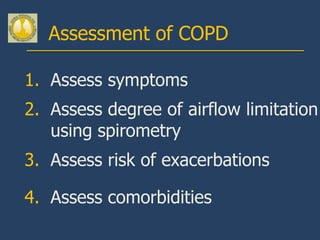
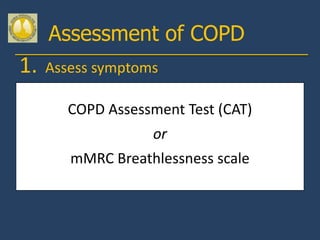
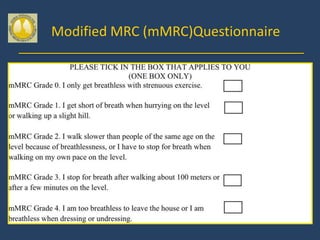
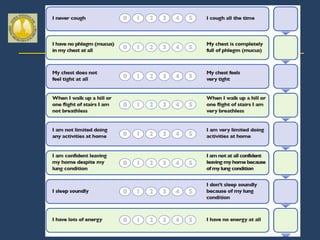
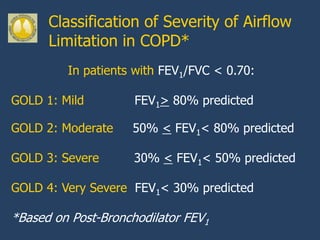
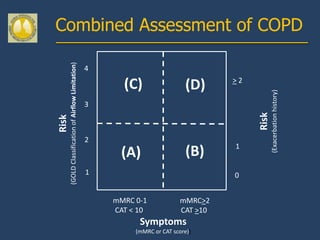
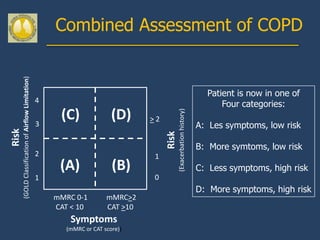
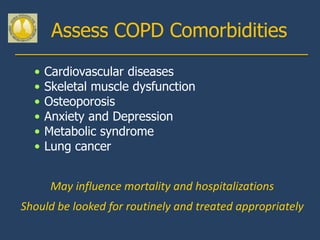
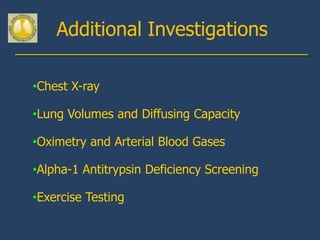
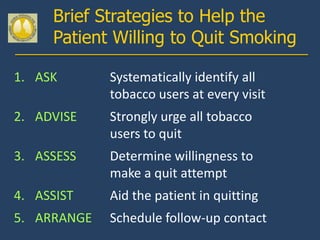
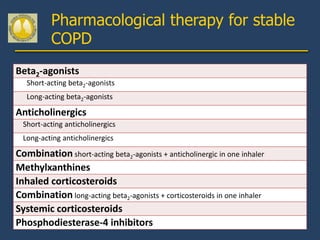
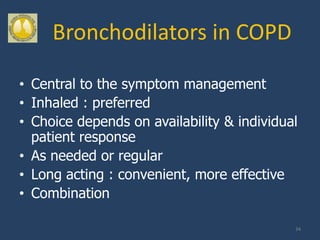
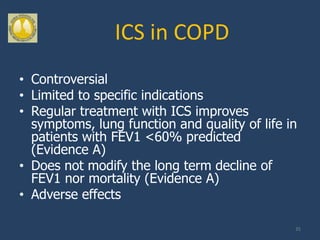
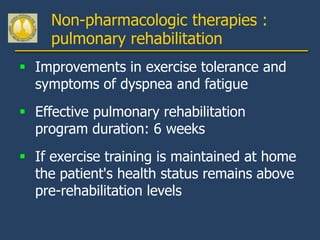
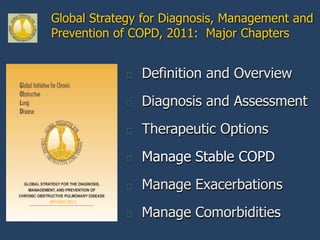
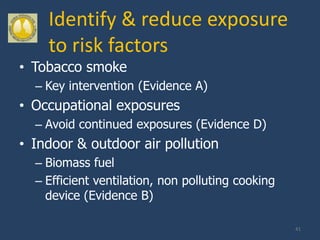
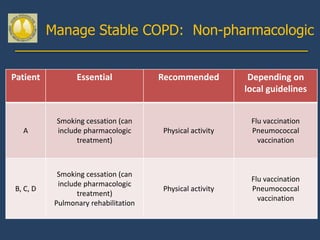
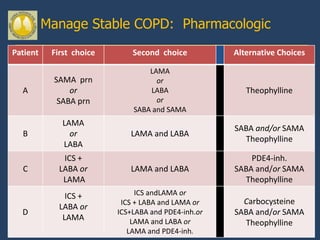
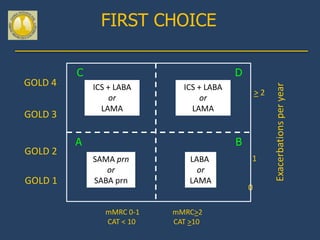
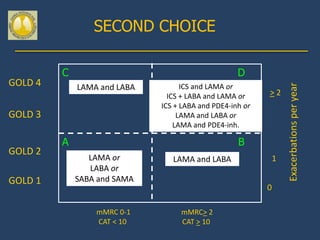
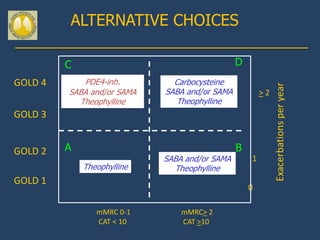
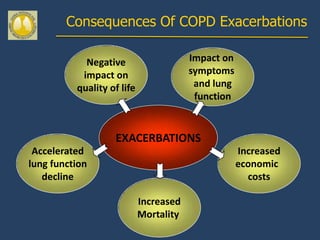
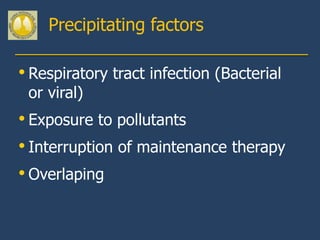
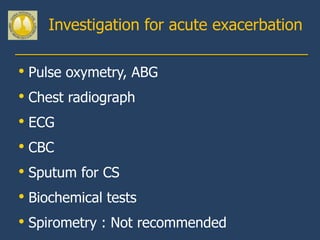
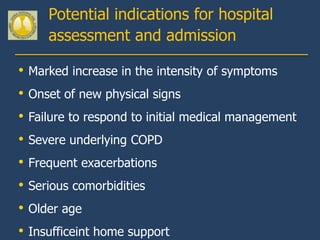
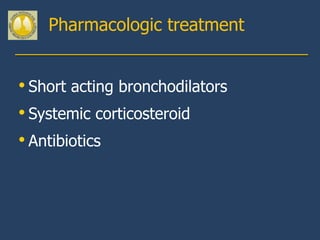
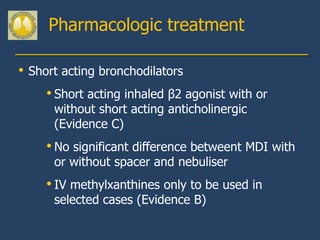
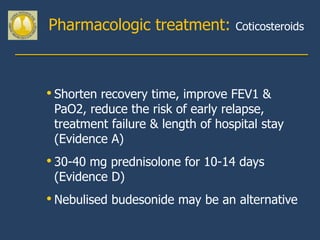
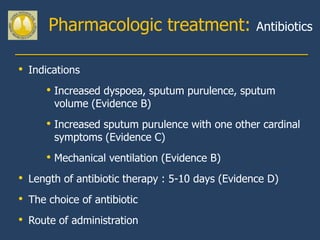
This document provides guidelines for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (COPD). It discusses COPD definitions and risk factors. The guidelines recommend assessing patients based on symptoms, spirometry results, exacerbation risk, and comorbidities. Treatment options include smoking cessation, bronchodilators, pulmonary rehabilitation, oxygen therapy, and managing exacerbations and comorbidities. The guidelines provide an evidence-based framework for diagnosing and staging COPD severity, as well as treating stable COPD and acute exacerbations.