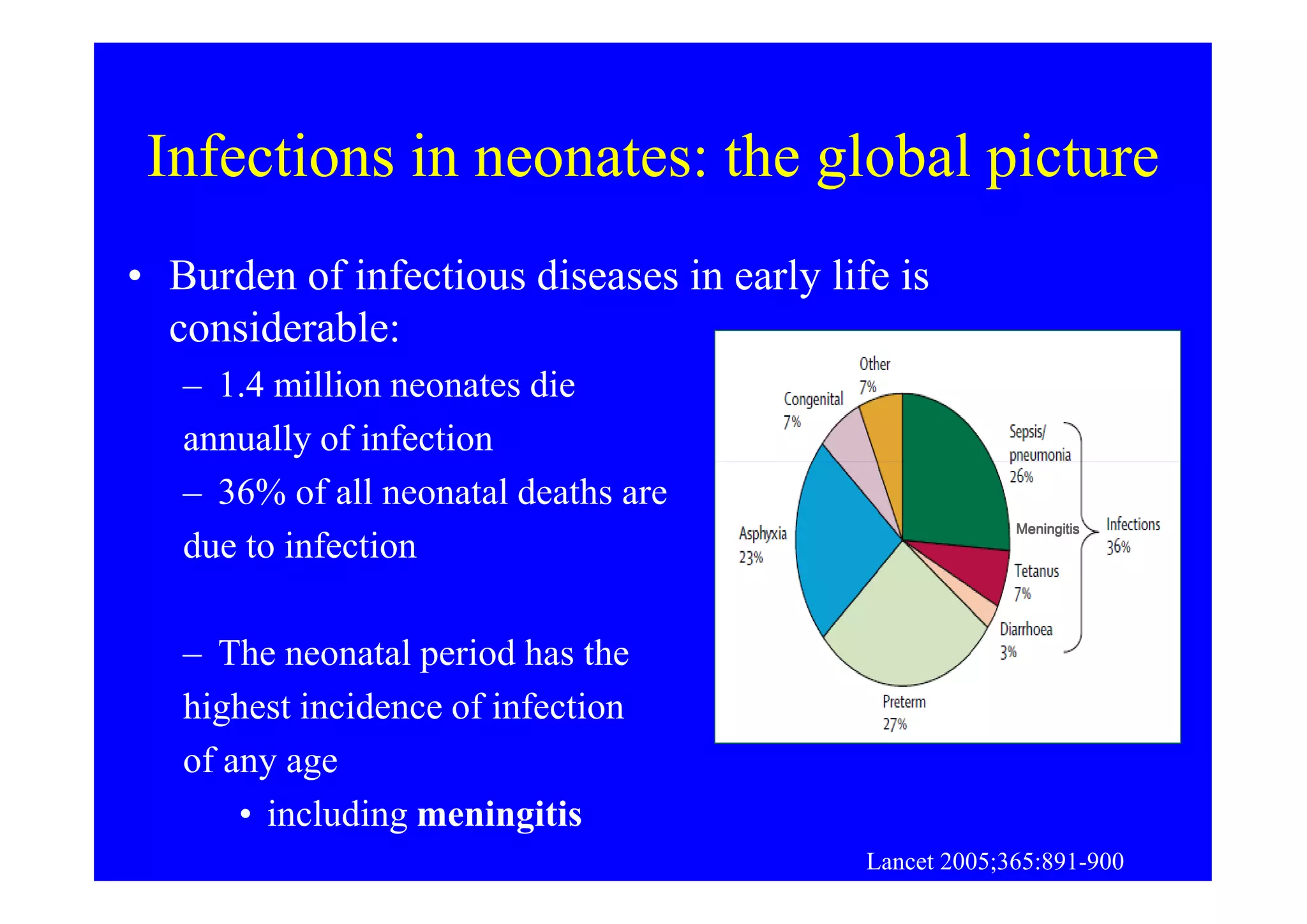
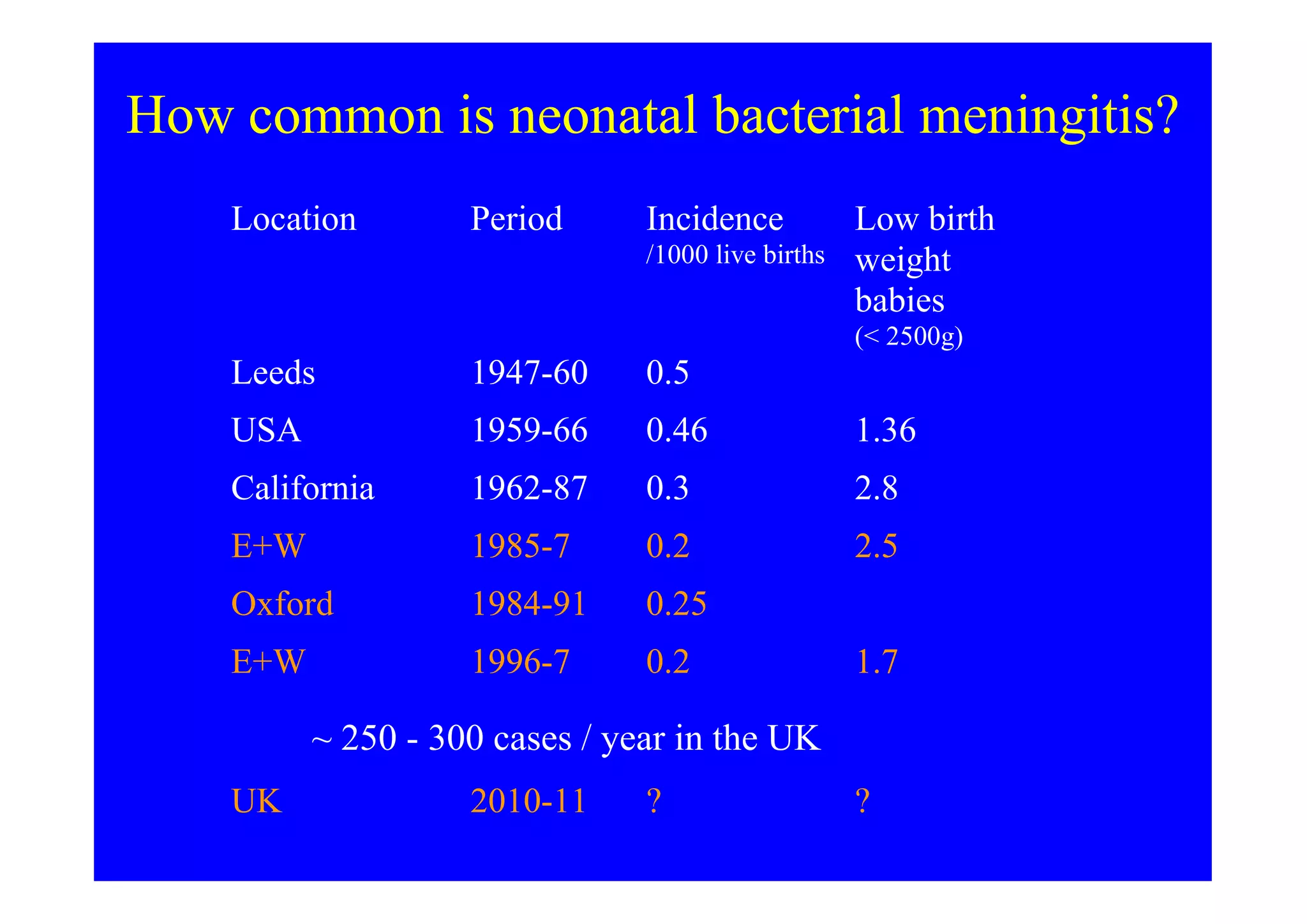
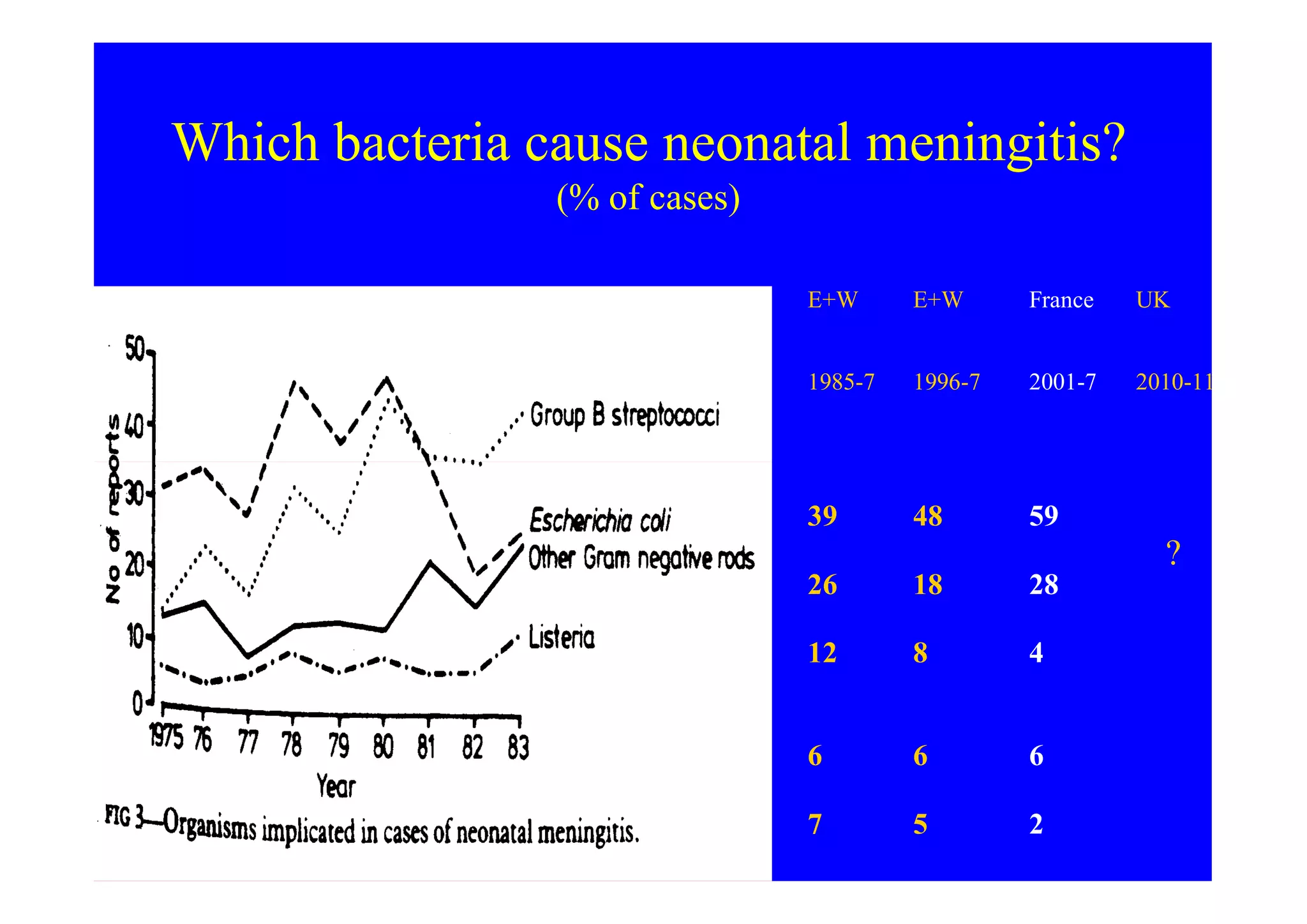
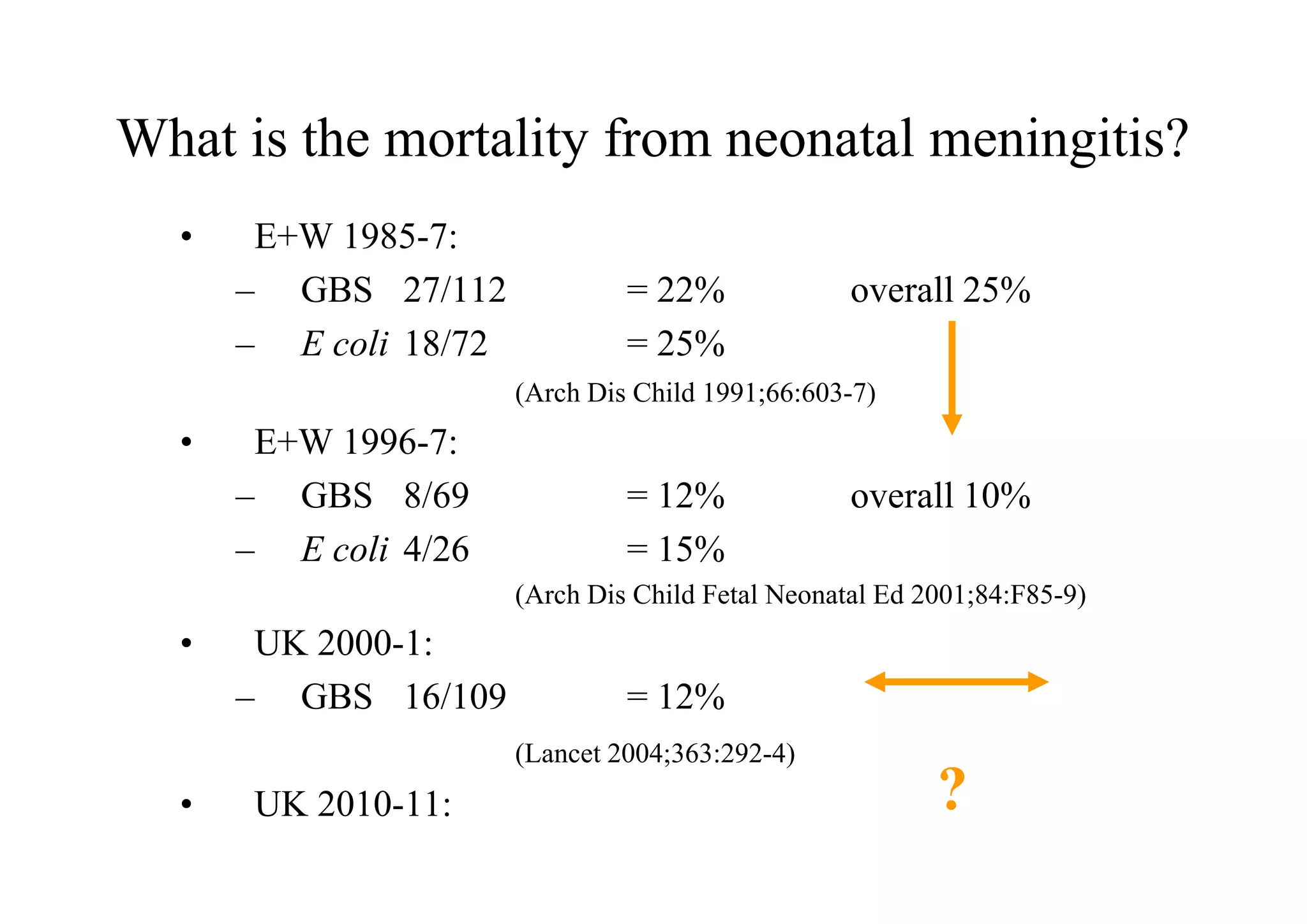
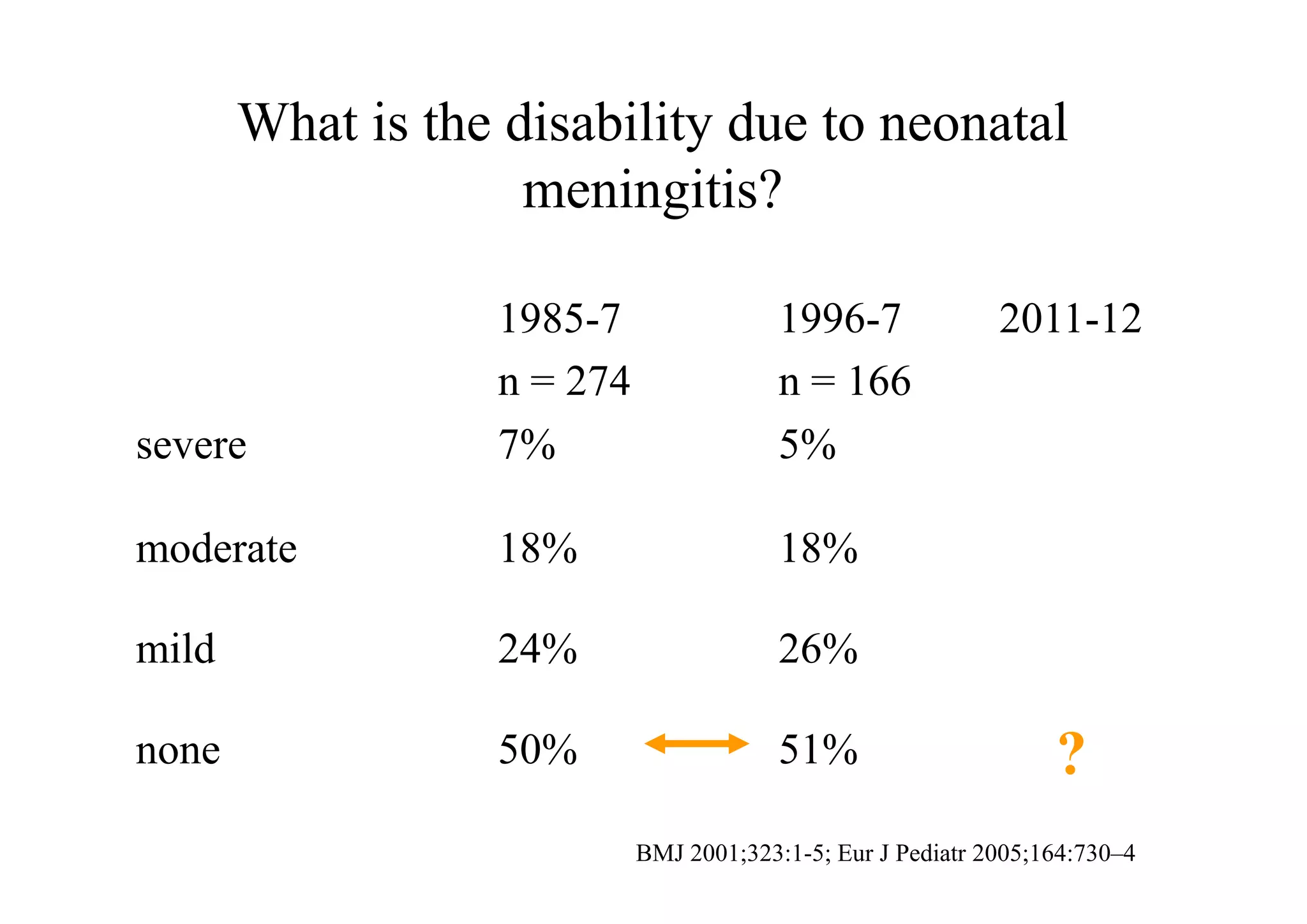
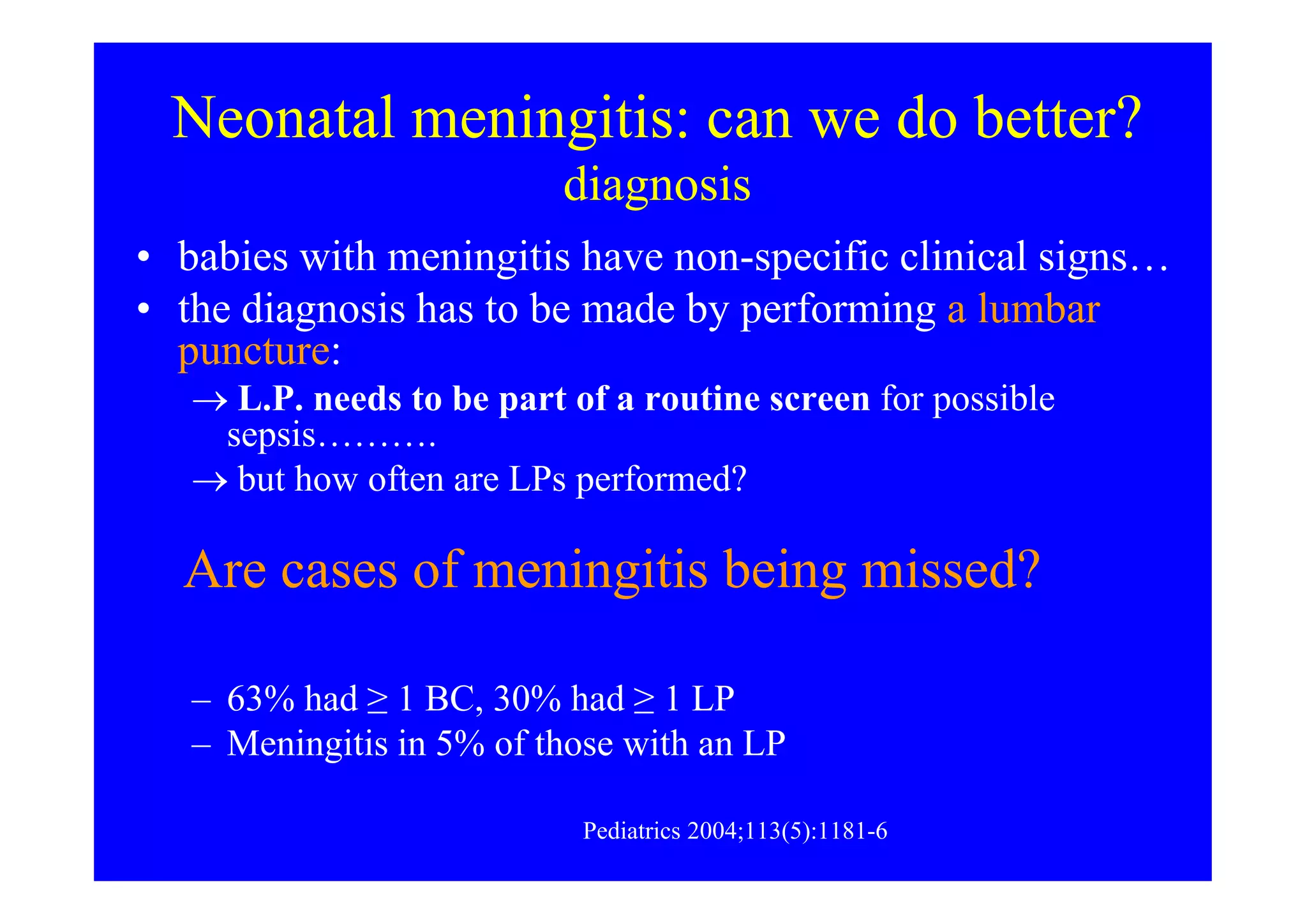
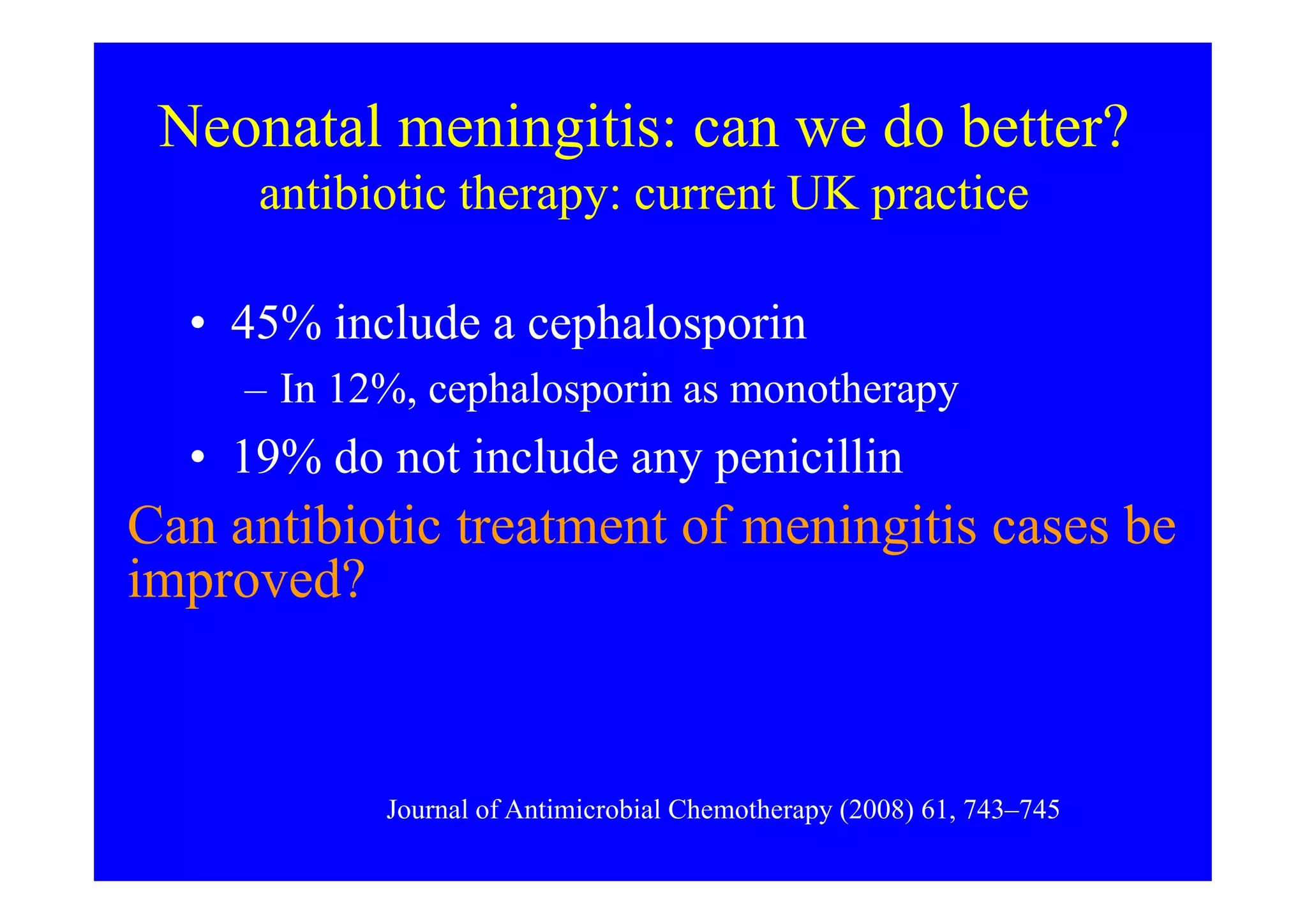
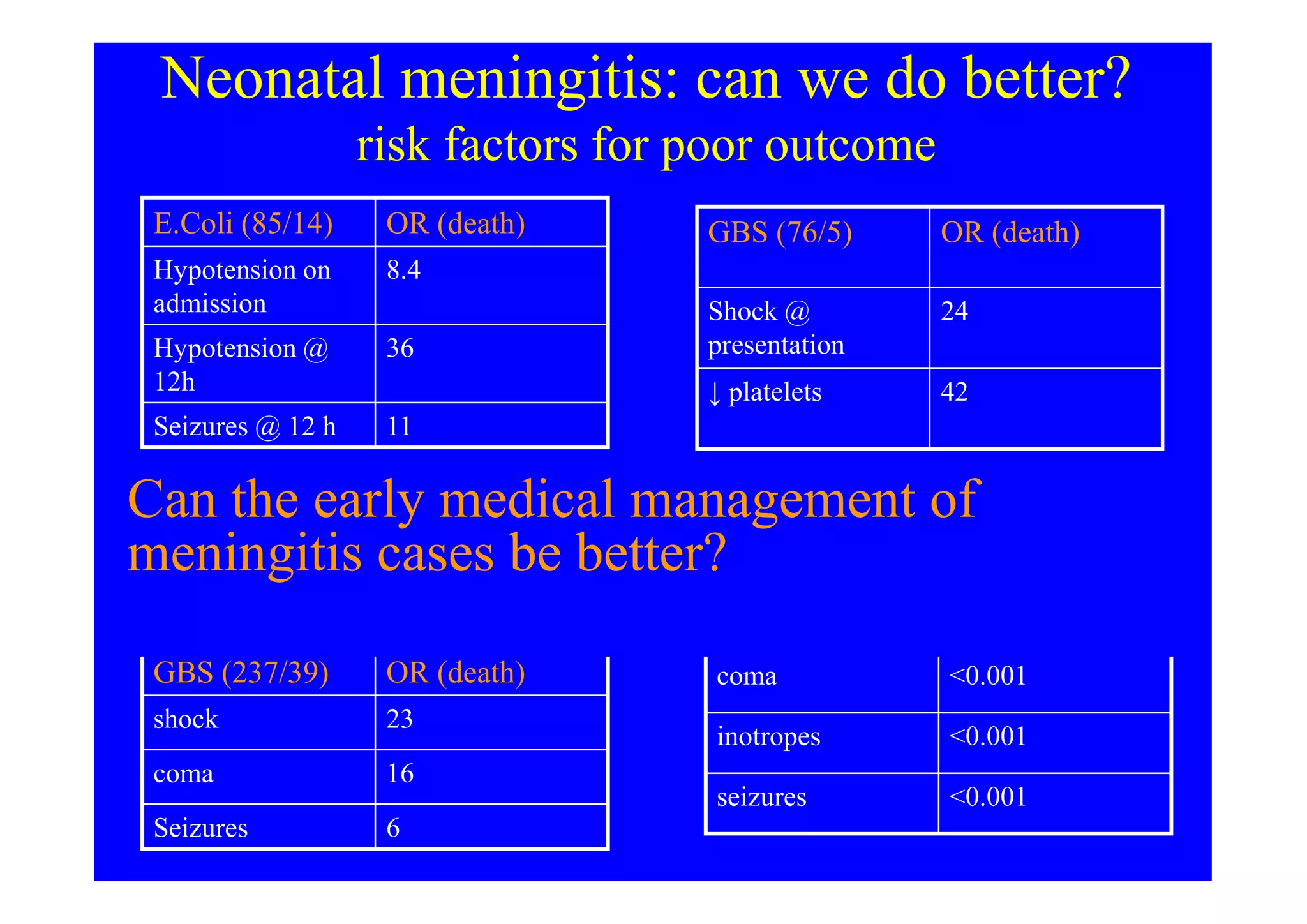
This document discusses neonatal meningitis and outlines opportunities to improve outcomes. It notes that 1) neonatal meningitis is a significant global cause of infant mortality, with Group B Streptococcus and E. coli as leading causes; 2) current UK mortality rates are 10-12% but management may be suboptimal; and 3) a new study aims to define the current burden of neonatal meningitis and identify ways to improve outcomes through earlier diagnosis, optimal antibiotic use, and supportive care.