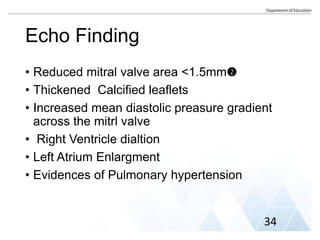
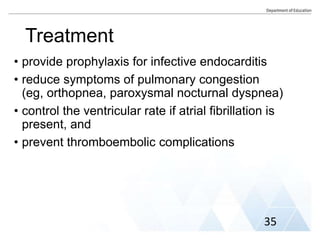
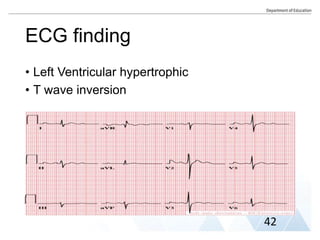
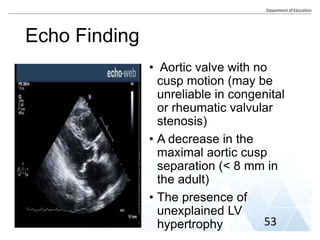
This document is a group assignment submitted by three nursing students on cardiovascular nursing care. It includes an outline on various heart valve diseases like mitral valve prolapse, mitral stenosis, aortic valve regurgitation, and aortic valve stenosis. For each condition, the summary discusses causes, symptoms, risk factors, complications, diagnostic findings, and nursing management. The assignment demonstrates the students' understanding of valvular heart diseases and aims to familiarize them with cardiovascular nursing care.





![• Assess mental status (Restlessness, severe anxiety,
and confusion).
• Check vital signs (heart rate and blood pressure).
• Assess heart sounds, noting gallops, S3, S4.
• Assess manually peripheral pulses (with weak rate,
rhythm indicated low cardiac output).
• Assess lung sounds and determine any occurrence
of Paroxysmal Nocturnal Dyspnea (PND) or
orthopnea.
• Monitor central venous, right arterial pressure [RAP],
pulmonary arterial pressure(PAP) Routinely
55](https://image.slidesharecdn.com/mitralandaorticvalvesfinal-230705224631-003cd8c7/85/Mitral-and-Aortic-Valves-Final-pptx-58-320.jpg)