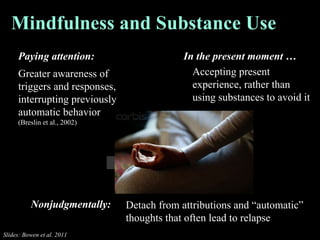
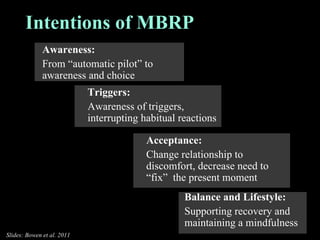
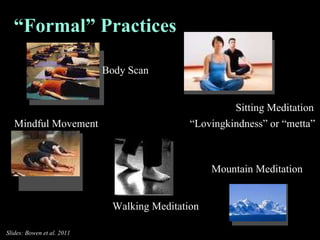
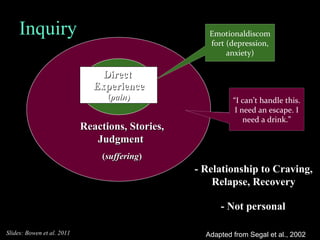
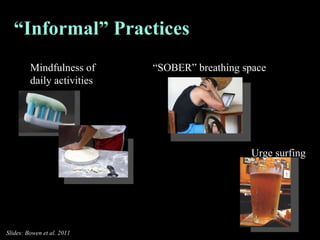
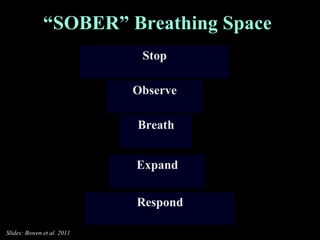
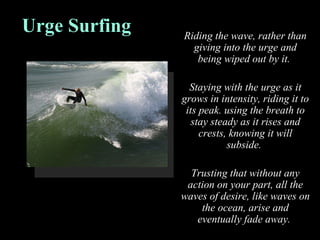
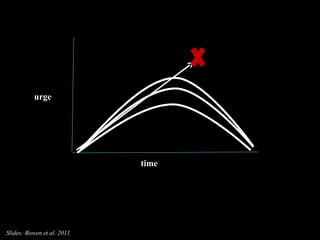
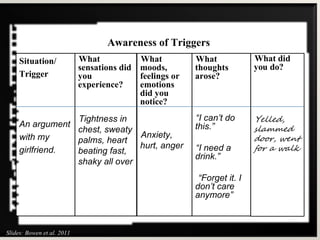
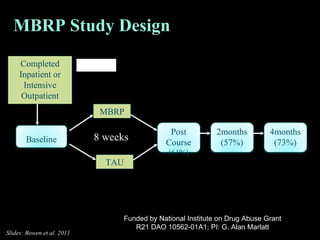
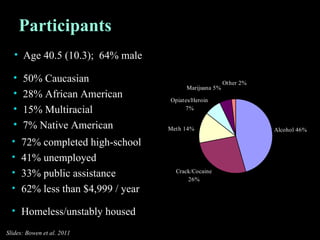
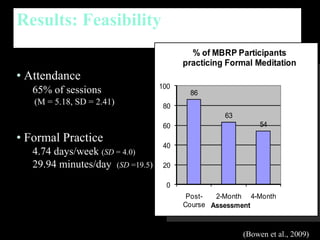
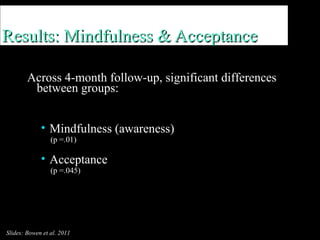
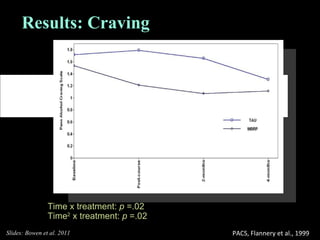
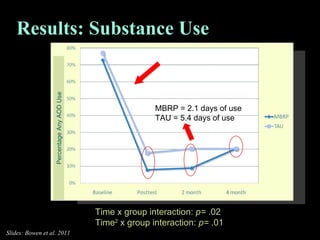
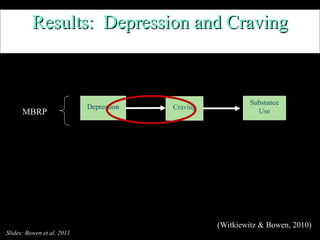
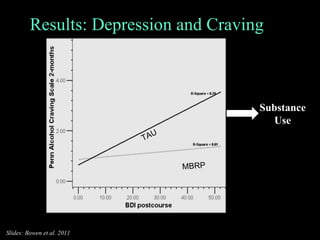
The document outlines the cognitive behavioral model of relapse and the effectiveness of relapse prevention therapy (RPT), including mindfulness-based relapse prevention (MBRP) as a treatment method. Research indicates that while RPT does not stop lapses more effectively than other treatments, it is better at delaying them and maintaining long-term treatment effects. MBRP integrates mindfulness practices to enhance awareness and acceptance, resulting in reduced craving and substance use among individuals with co-occurring disorders.