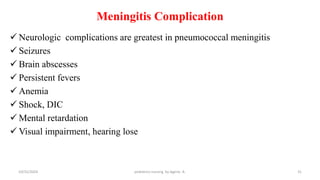
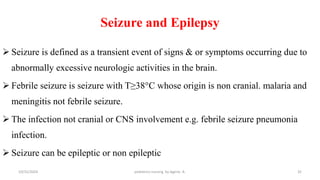
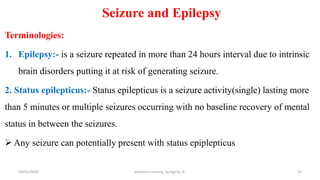
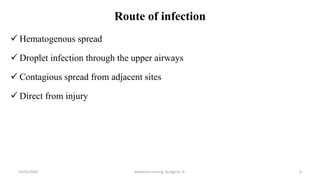
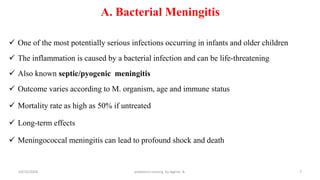
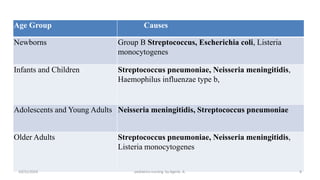
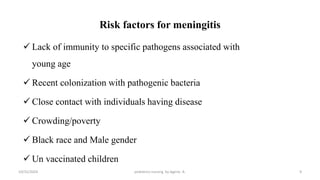
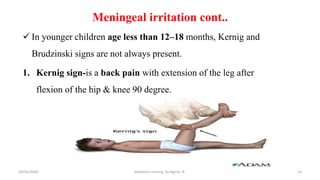
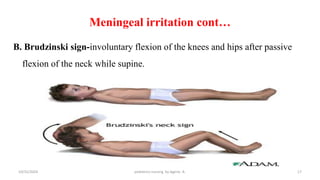
The document is a comprehensive educational presentation about pediatric neurologic infections and disorders aimed at third-year nursing students. It focuses primarily on meningitis, detailing its definitions, causes, clinical manifestations, diagnostic techniques, treatment protocols, and nursing care strategies. The presentation also covers seizures and epilepsy, explaining their classifications and pathophysiology.
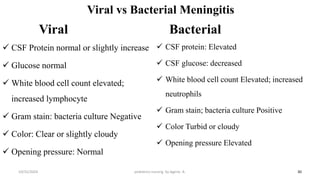
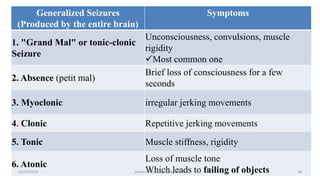
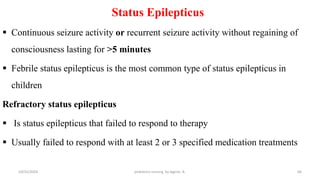
![Differential Diagnosis
Infection:
1. Generalized infection of the CNS
Bacteria [Tb meningitis, Syphilis]
Fungi [Histoplasma ,Candida…]
Viruses [Enteroviruses , HSV]
2. Focal infections of the CNS
Brain abscess, Para meningeal abscess
Non infectious diseases:
Malignancy, toxins
21
10/31/2024 pediatrics nursing by Agerie. A.](https://image.slidesharecdn.com/2-241203180408-c2229be9/85/2-Nursing-noteNeurological-disorders-pdf-21-320.jpg)