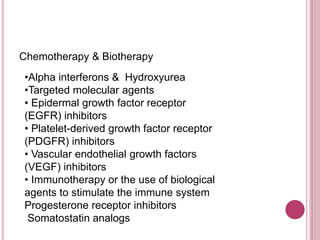
Meningiomas are tumors that arise from the meninges, the membranes surrounding the brain and spinal cord. They are usually benign and slow-growing, pressing on brain tissue and causing symptoms like headache. Meningiomas account for about 34% of all primary brain tumors and occur more often in older adults and women. While surgery is often the first treatment, some meningiomas require radiation or other therapies like anti-seizure medications, steroids, or targeted molecular agents depending on their characteristics and response to initial treatment.