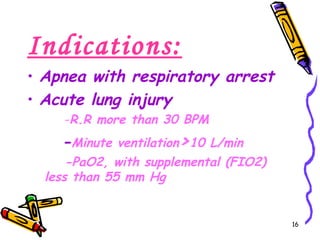
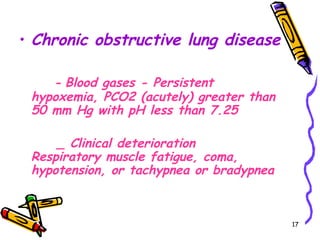
The document discusses mechanical ventilation, including its history, definitions, classifications, indications, physiologic aspects, ventilator modes, complications, and weaning process. Mechanical ventilation uses specially designed pumps to support respiratory function through application of high oxygen gas and positive pressure. Modes discussed include assist control, SIMV, CPAP, PCV, and PSV, with complications including barotrauma, pneumonia, and respiratory muscle deconditioning.