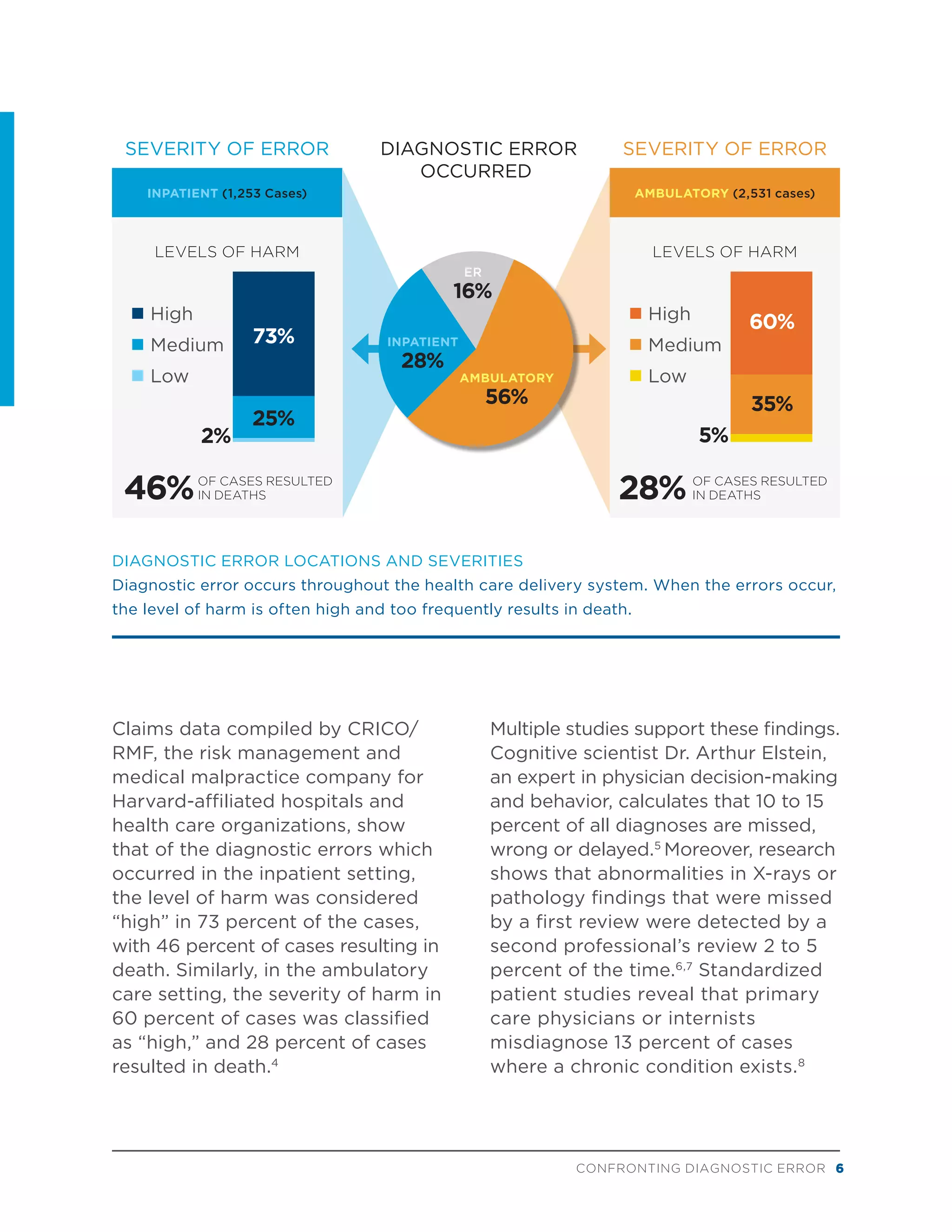
The document discusses diagnostic error in healthcare. It begins by noting that inaccurate diagnoses, incorrect treatments, and lack of diagnoses contribute to unnecessary costs, inefficiency, and patient dissatisfaction. Improving diagnostic accuracy can help achieve quality, control costs, and increase patient satisfaction. The document then discusses:
- The high incidence of diagnostic errors, which result in tens of thousands of deaths per year and enormous financial tolls.
- Evidence that diagnostic errors commonly cause patient harm and occur across primary care, inpatient, and outpatient settings.
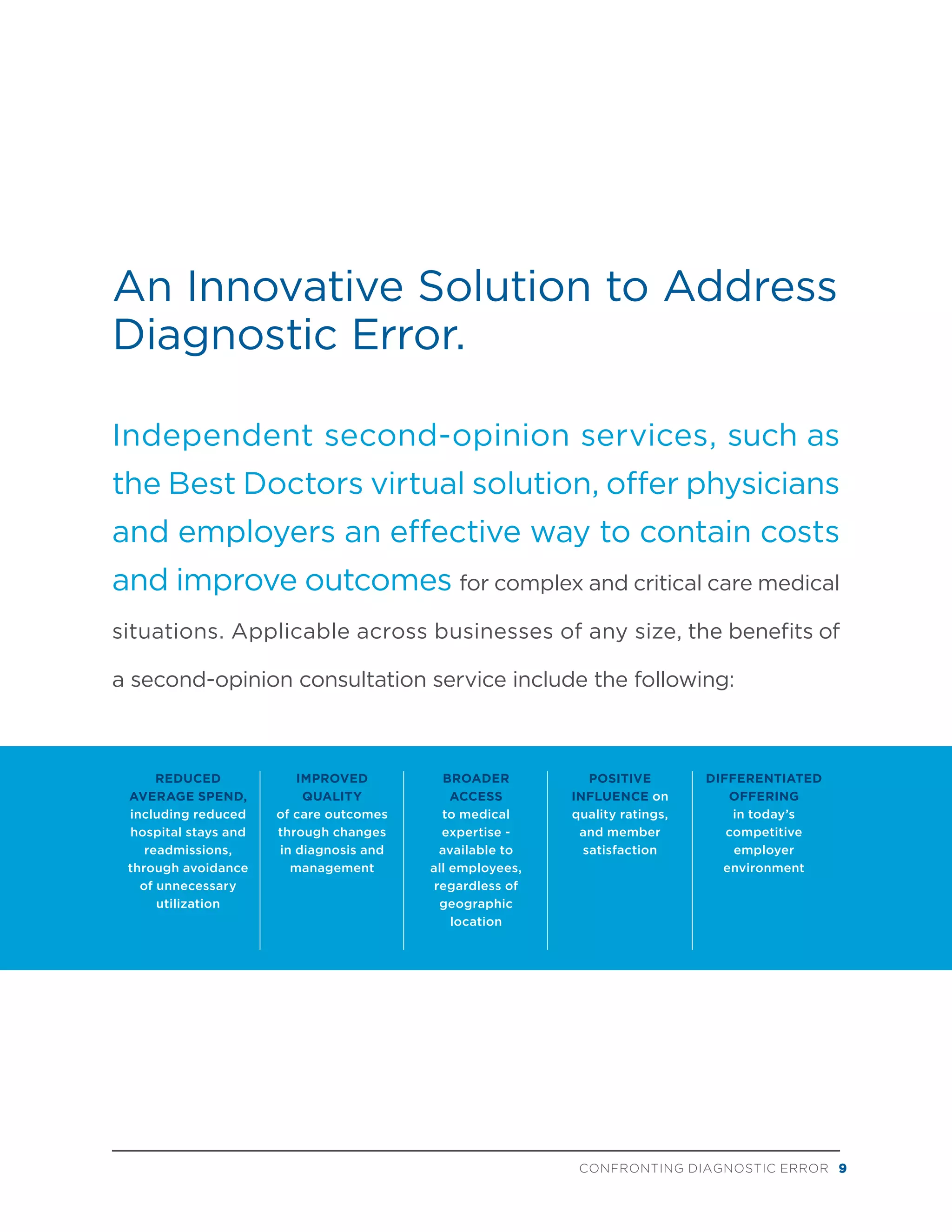
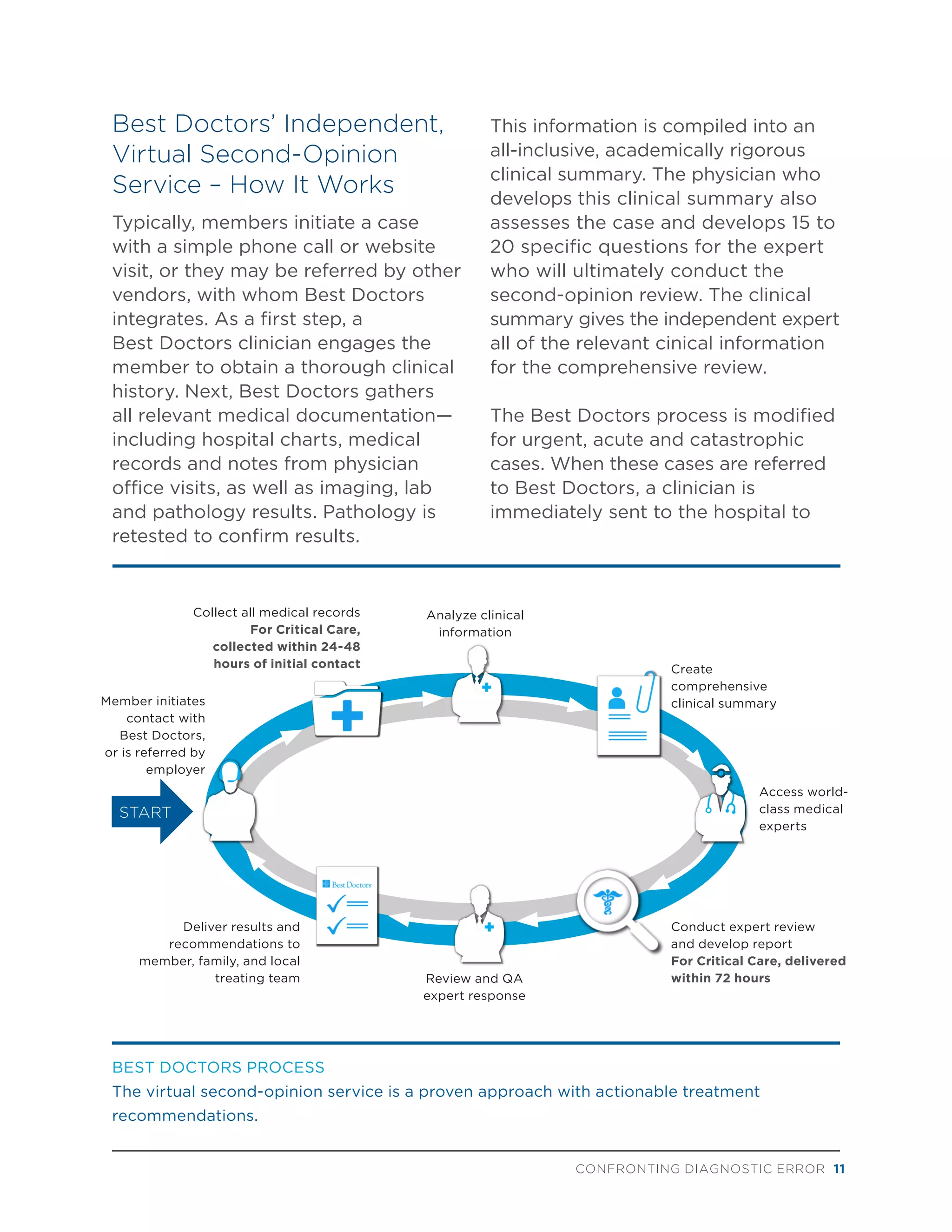
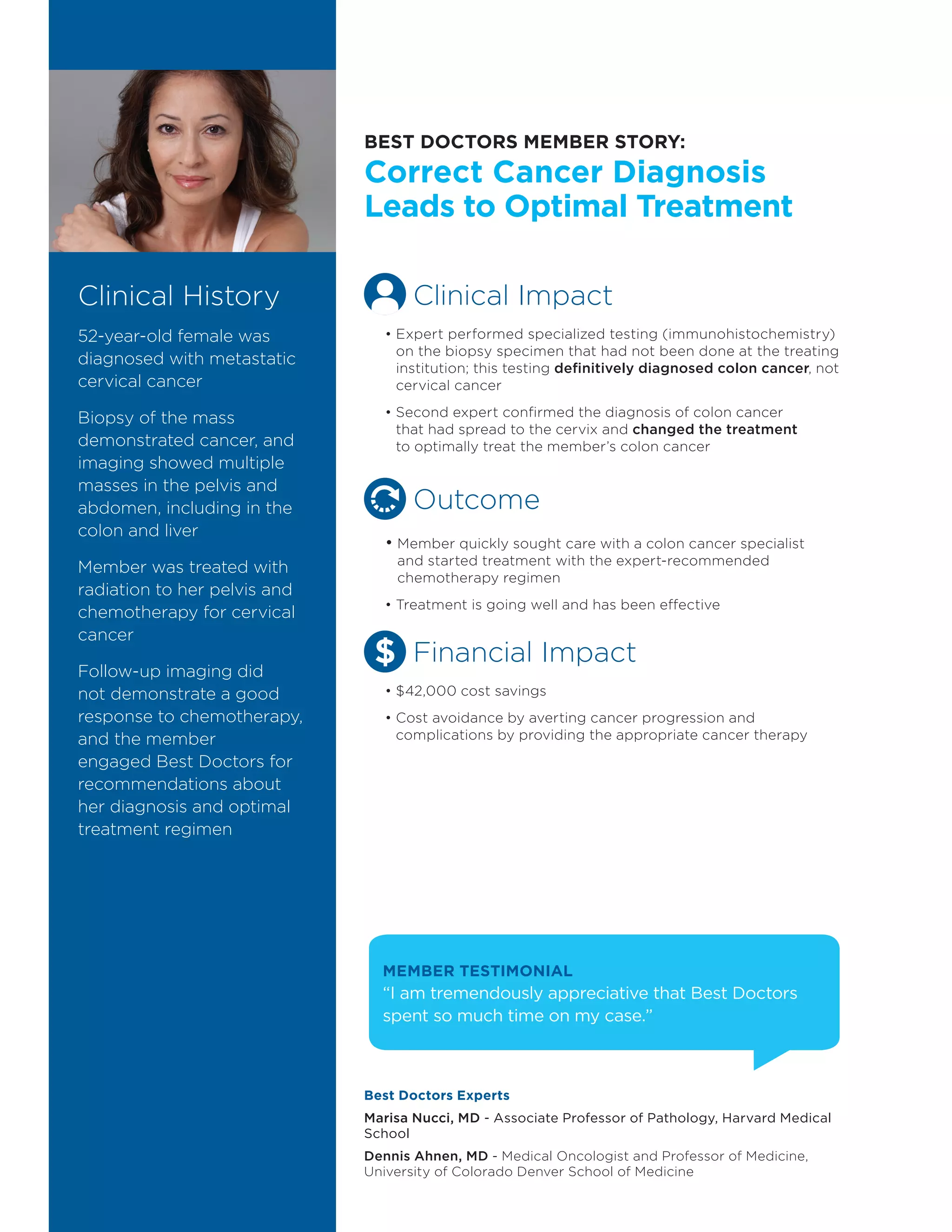
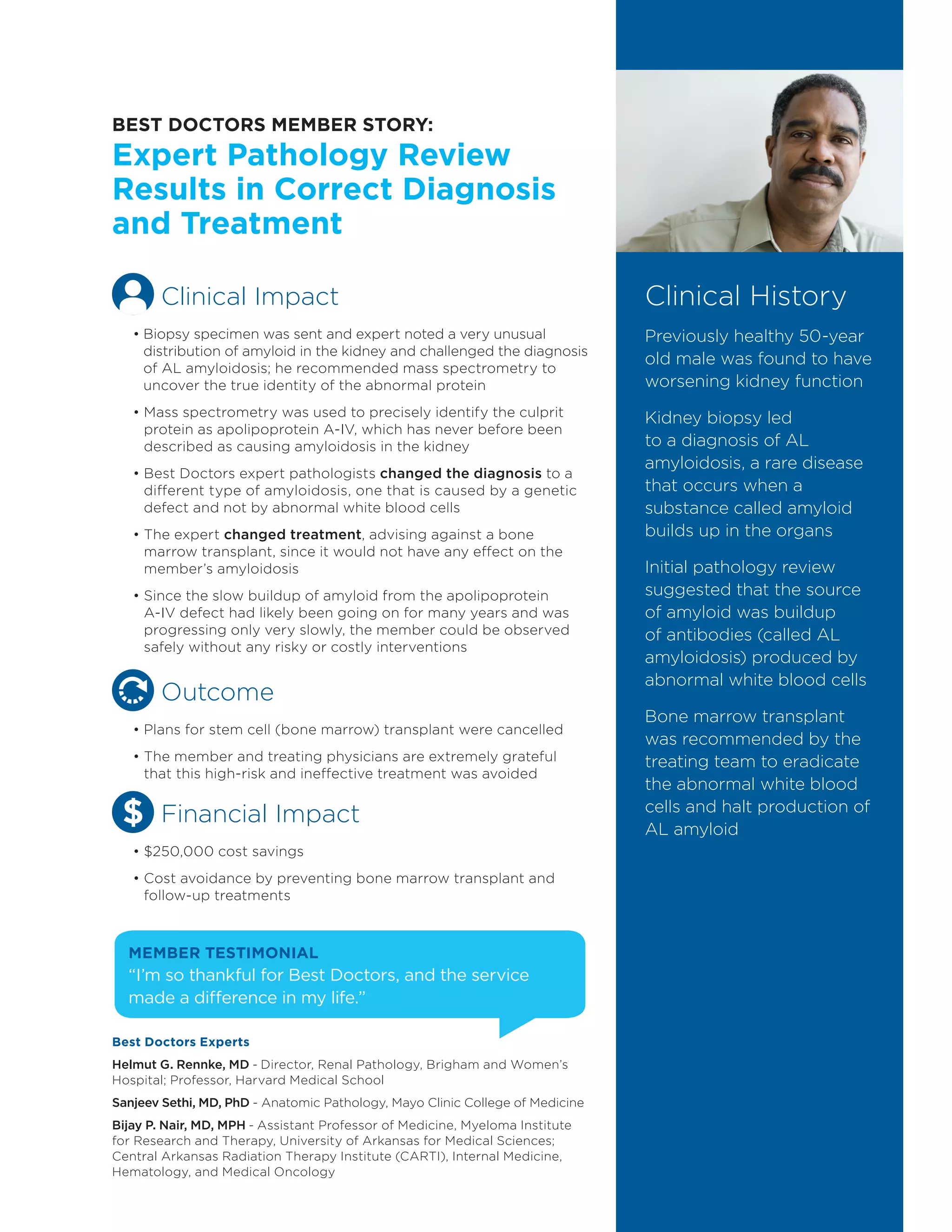
- An innovative solution of independent virtual second opinions to address diagnostic errors by improving accuracy and ensuring appropriate treatment.