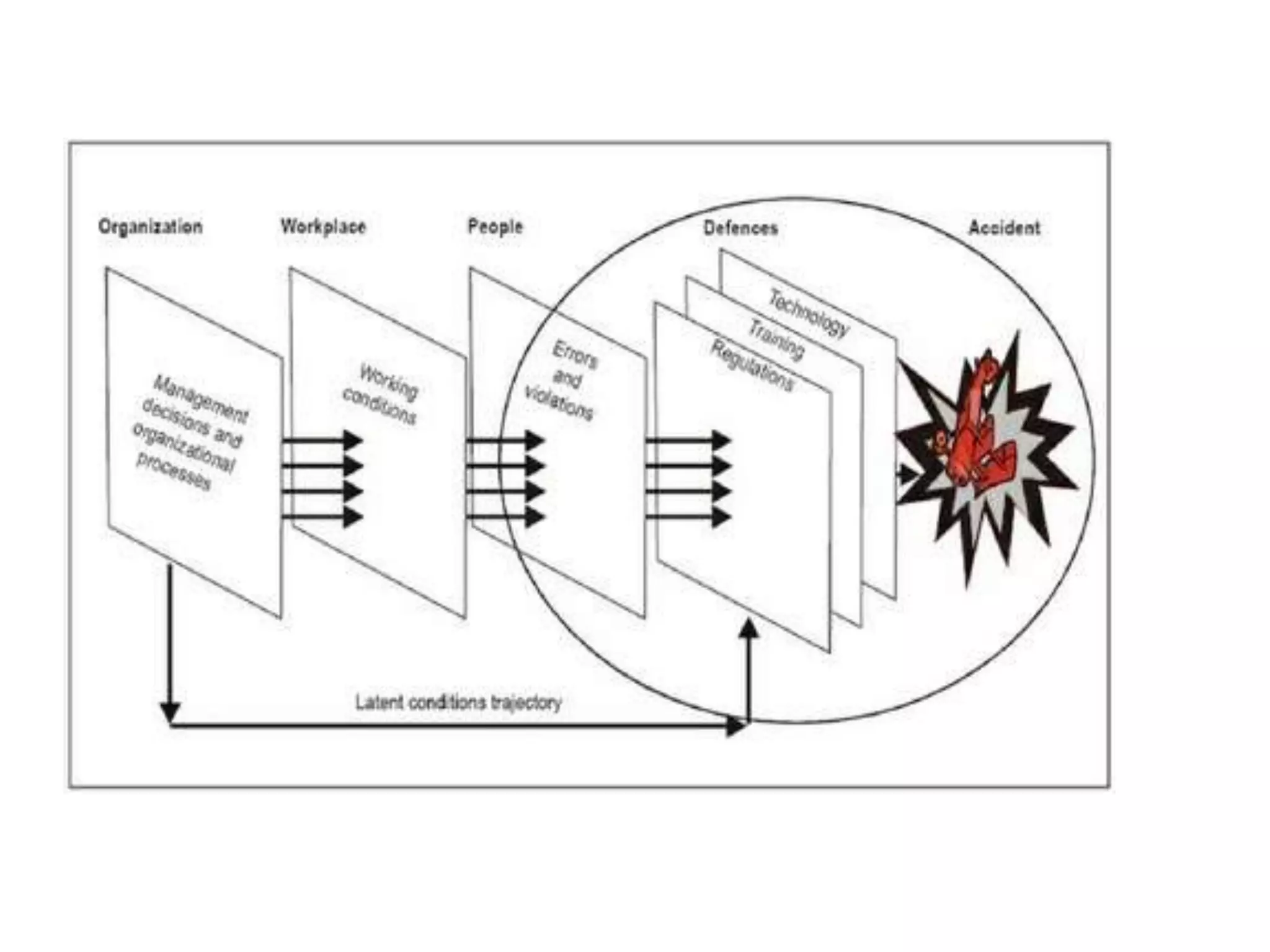
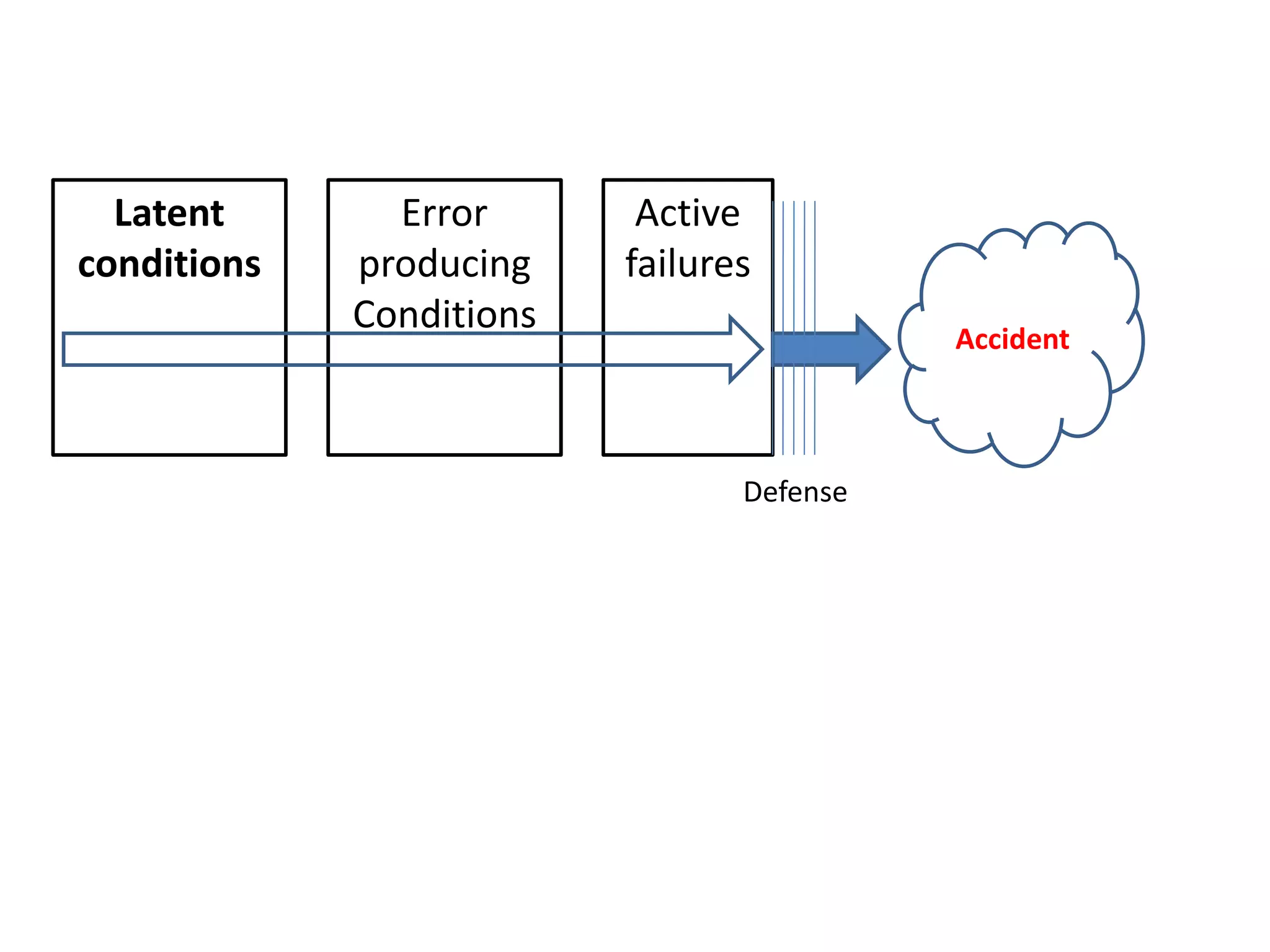
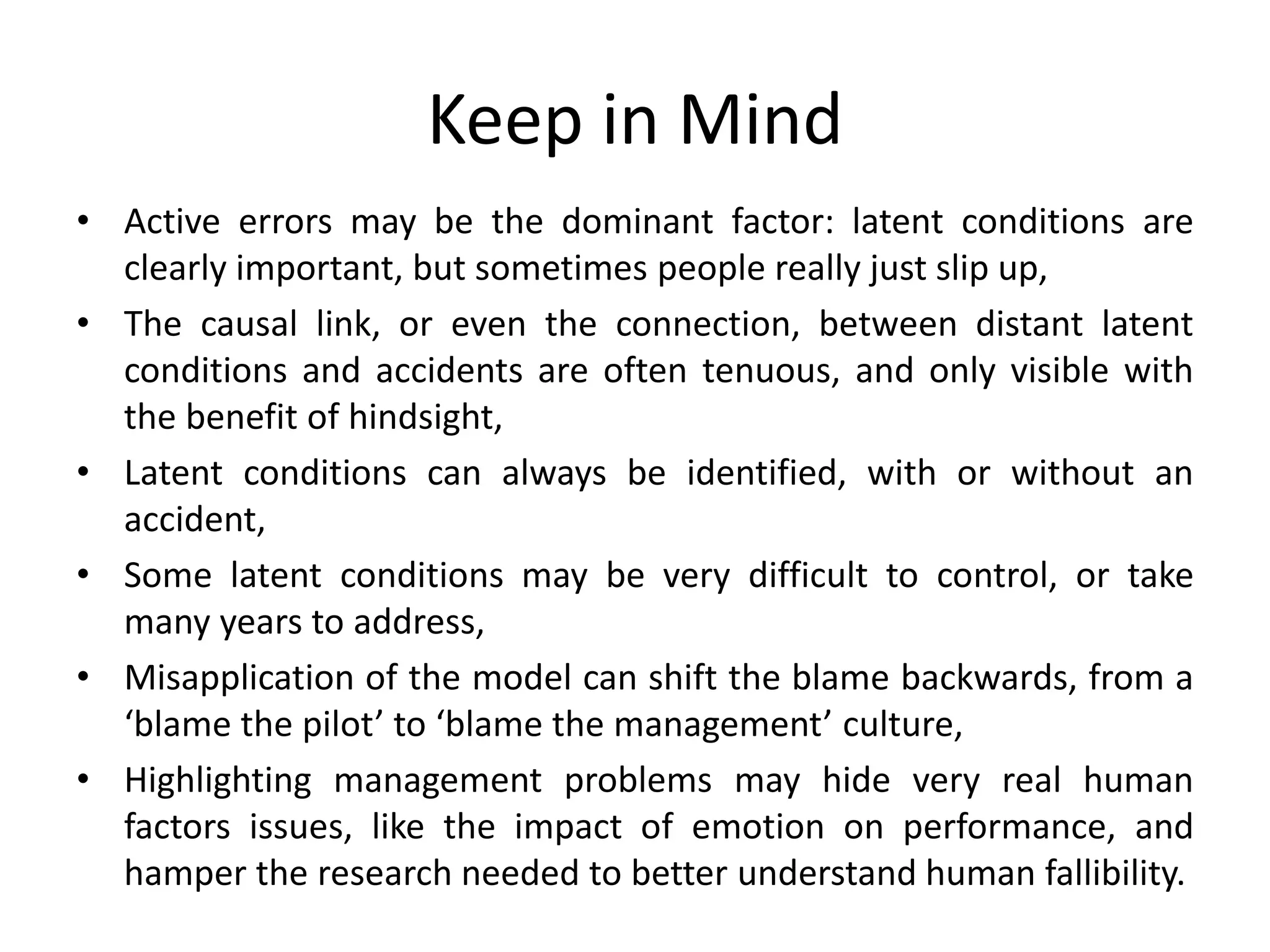
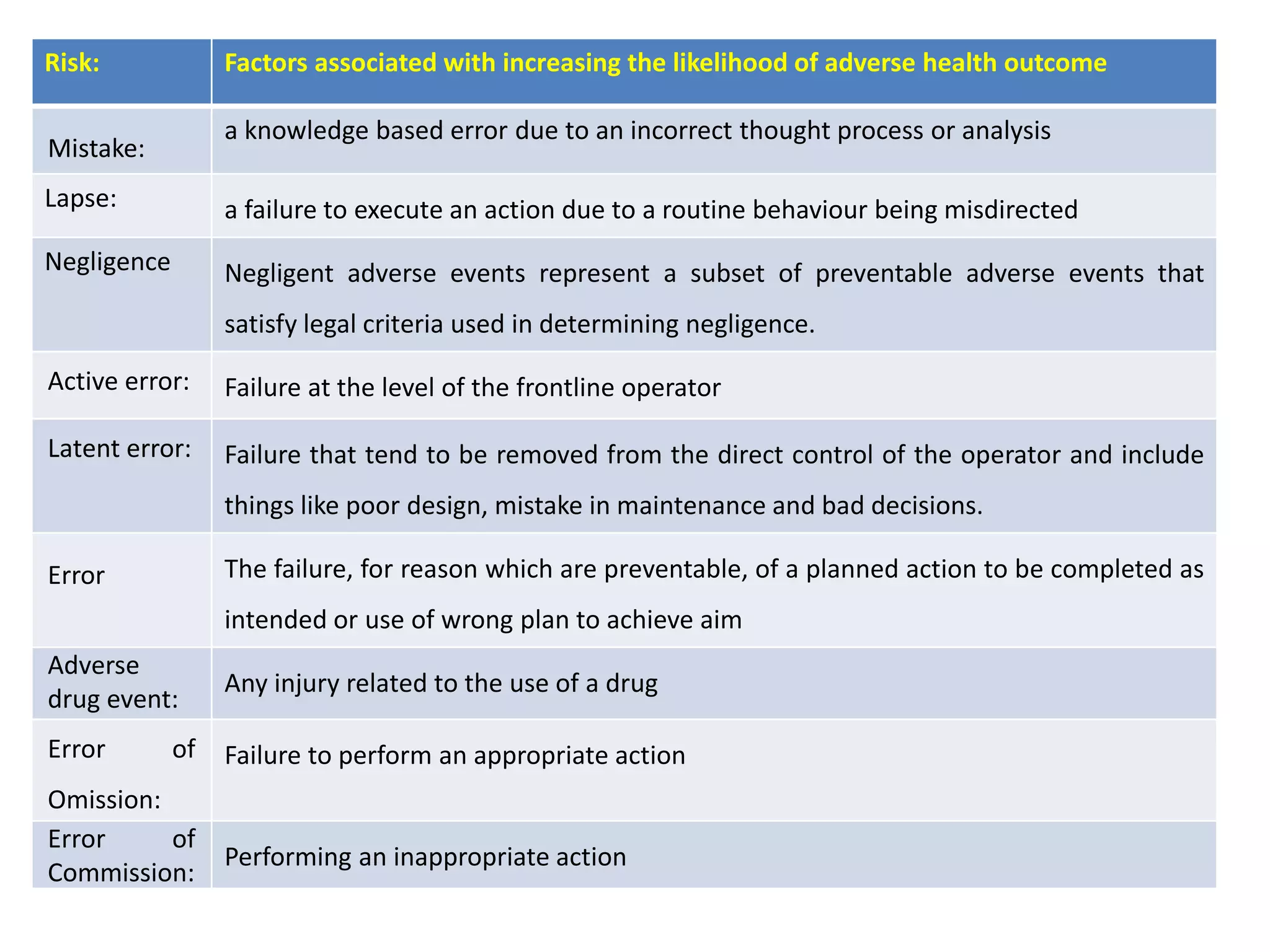
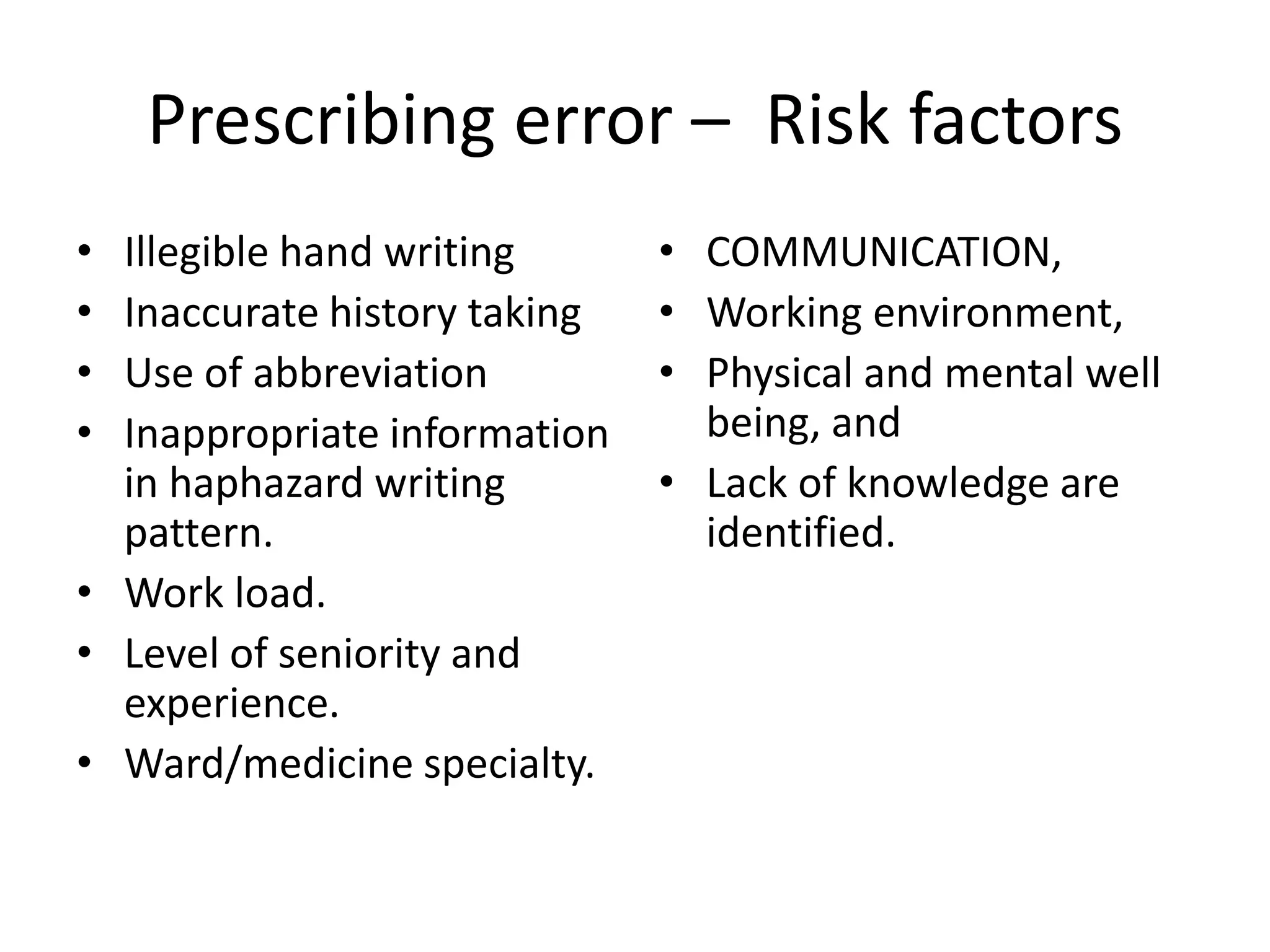
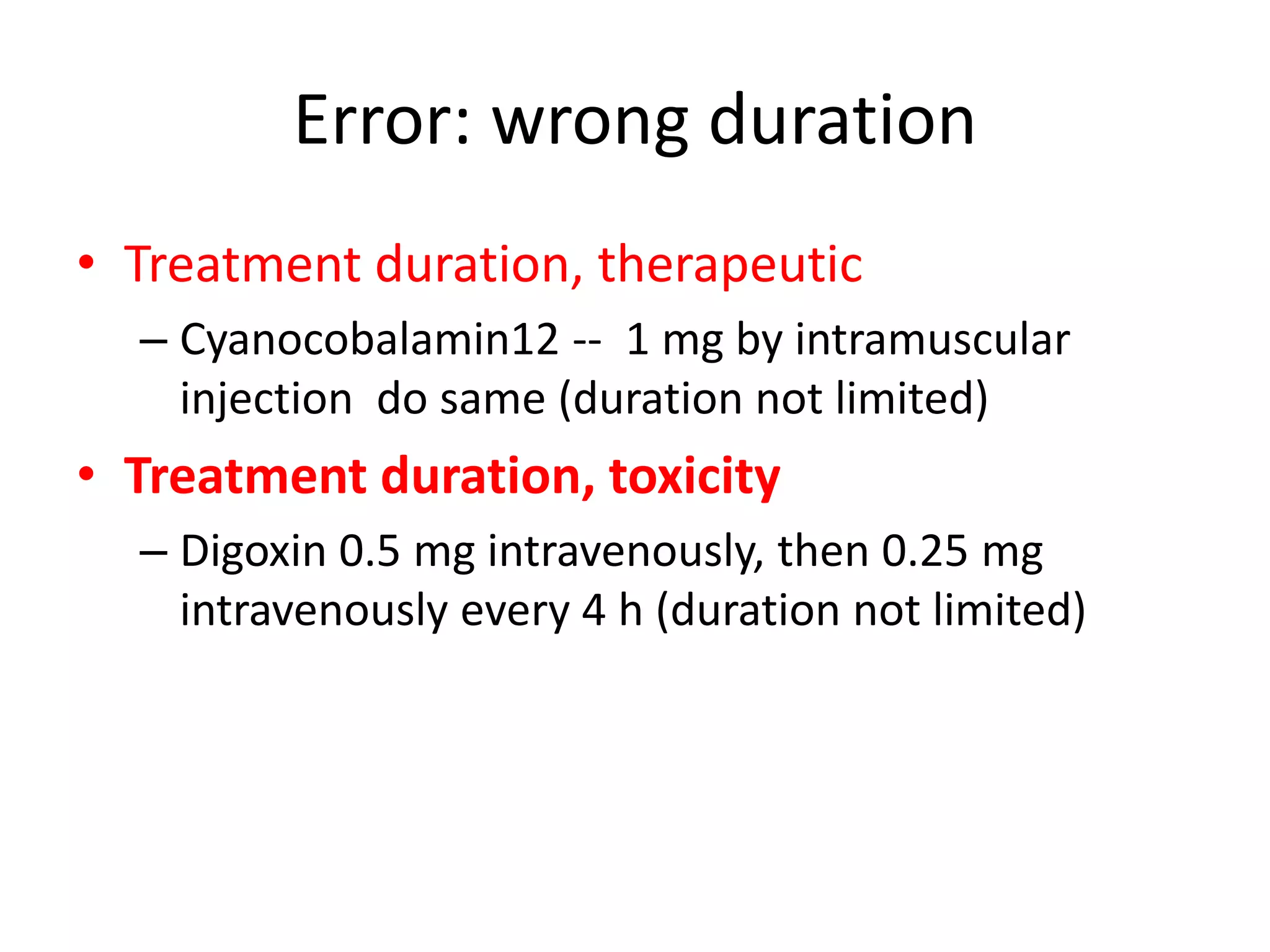
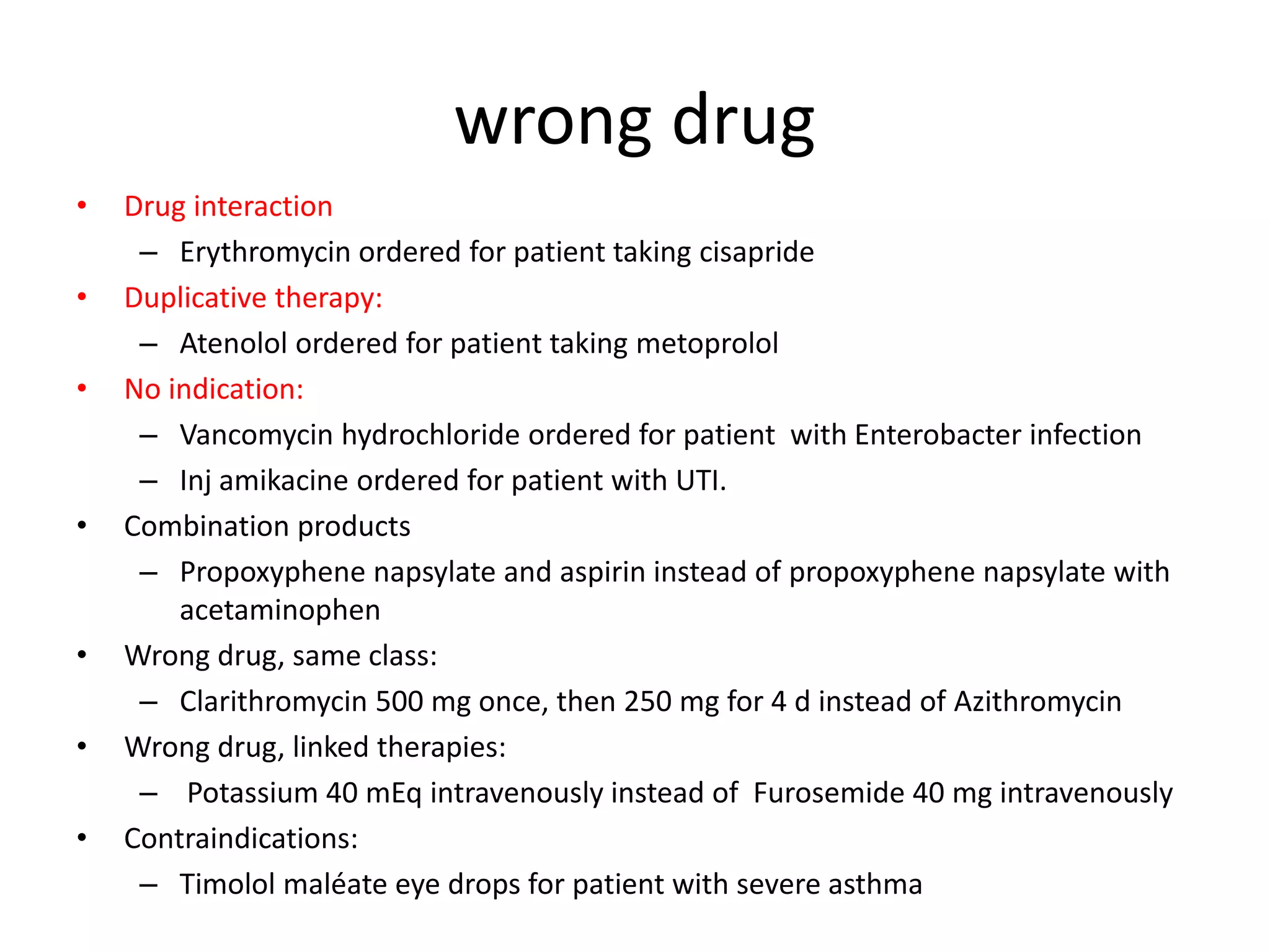
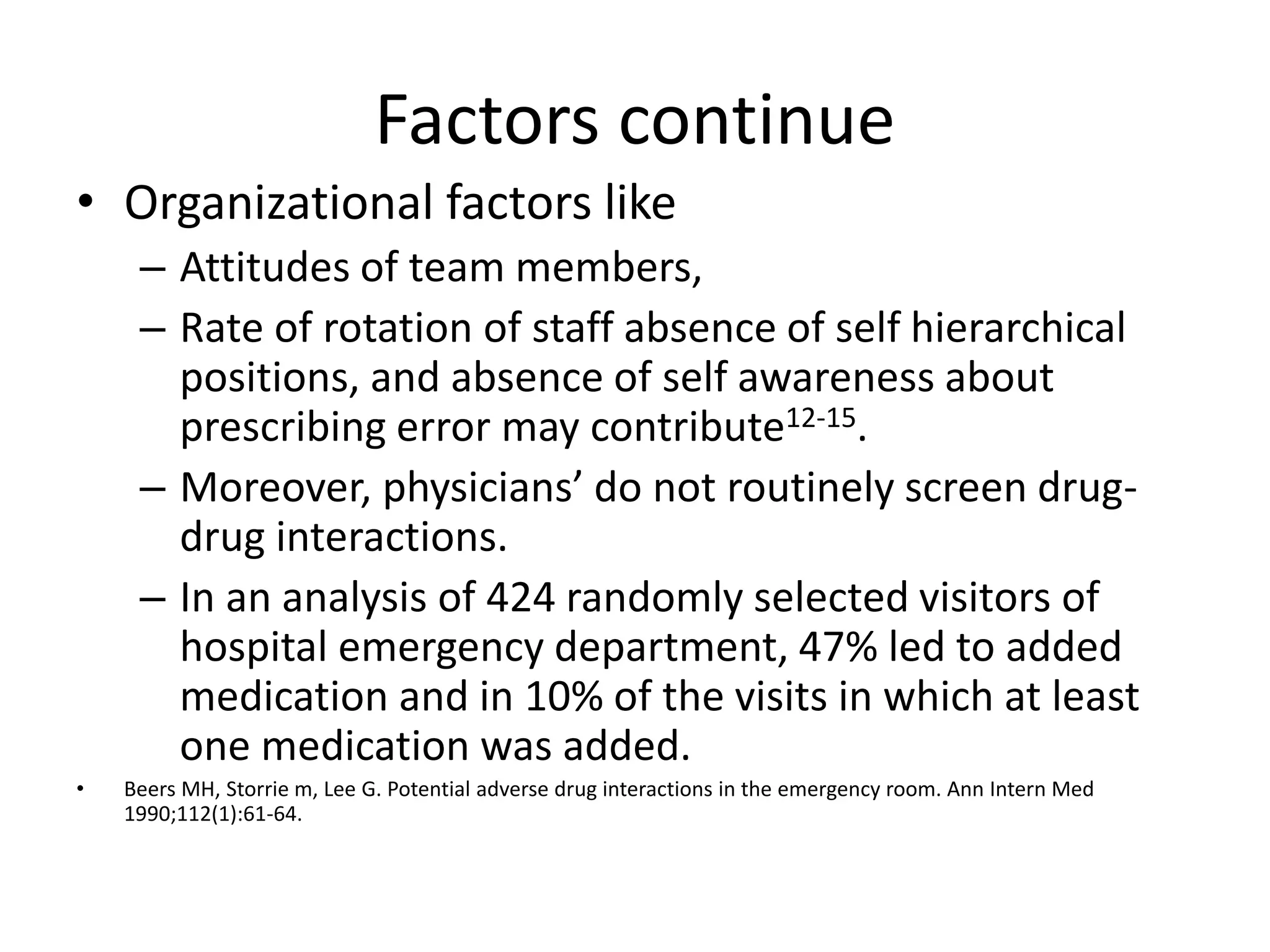
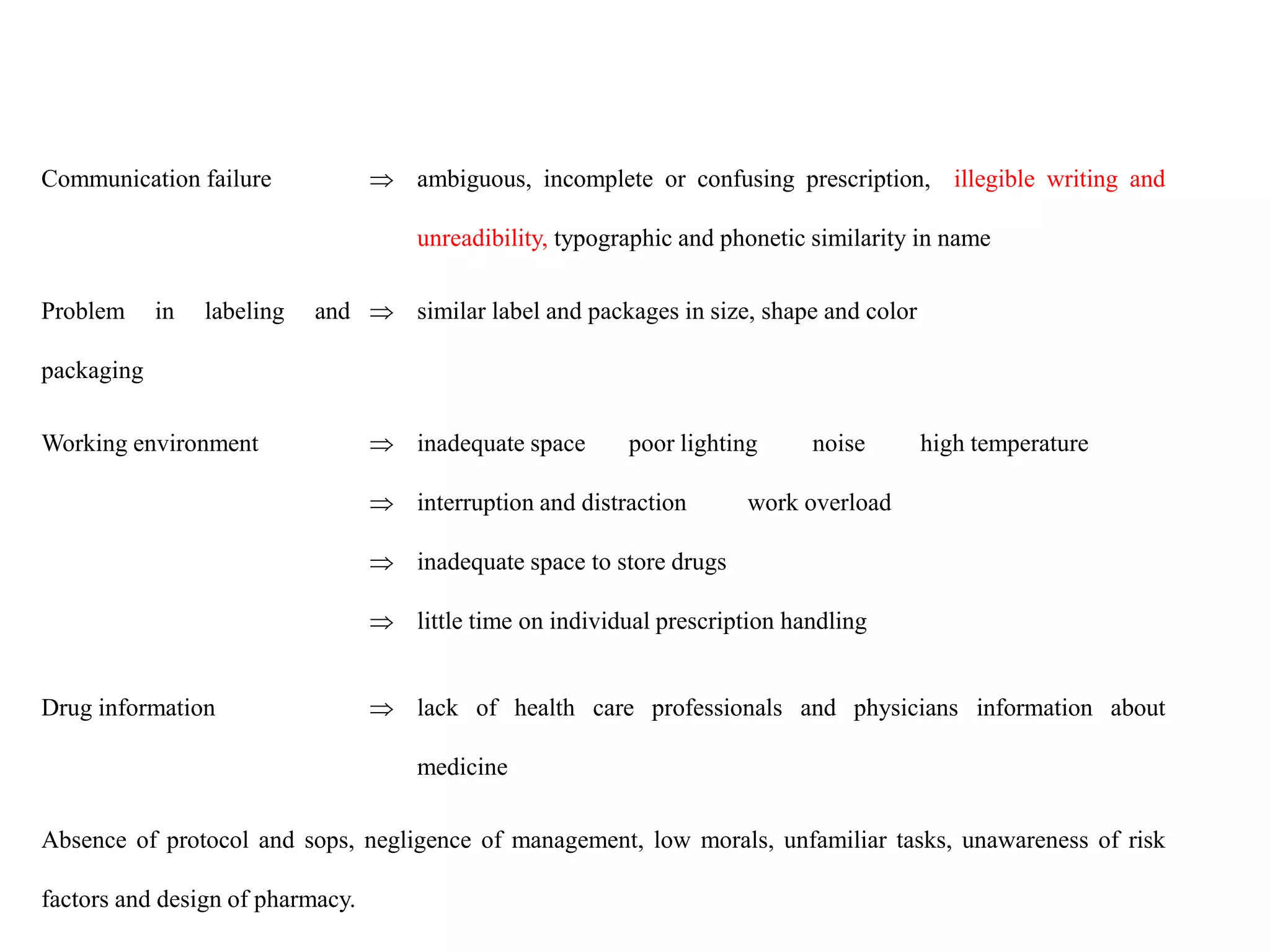
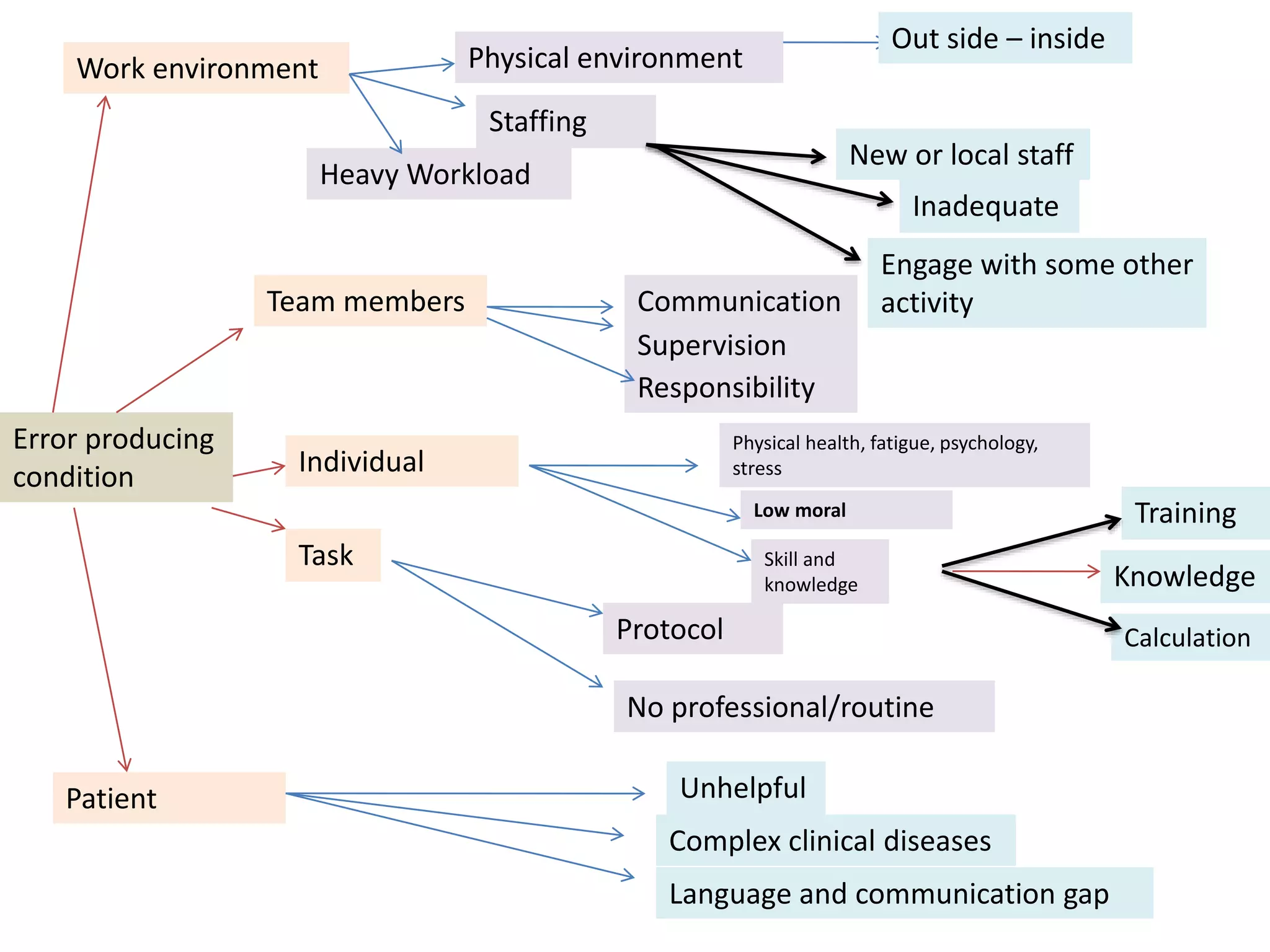
Medication errors are a significant problem in healthcare that can harm patients. They occur commonly at various stages of the medication process including prescribing, transcribing, preparing, dispensing, and administering medications. Several studies over decades have found high rates of medication errors and preventable adverse drug events in hospitals. James Reason developed a widely used model for classifying errors as either active failures by frontline staff or latent failures due to upstream organizational or management issues. Understanding the causes of errors through models like Reason's can help pharmacists and other healthcare providers develop effective strategies to improve medication safety.
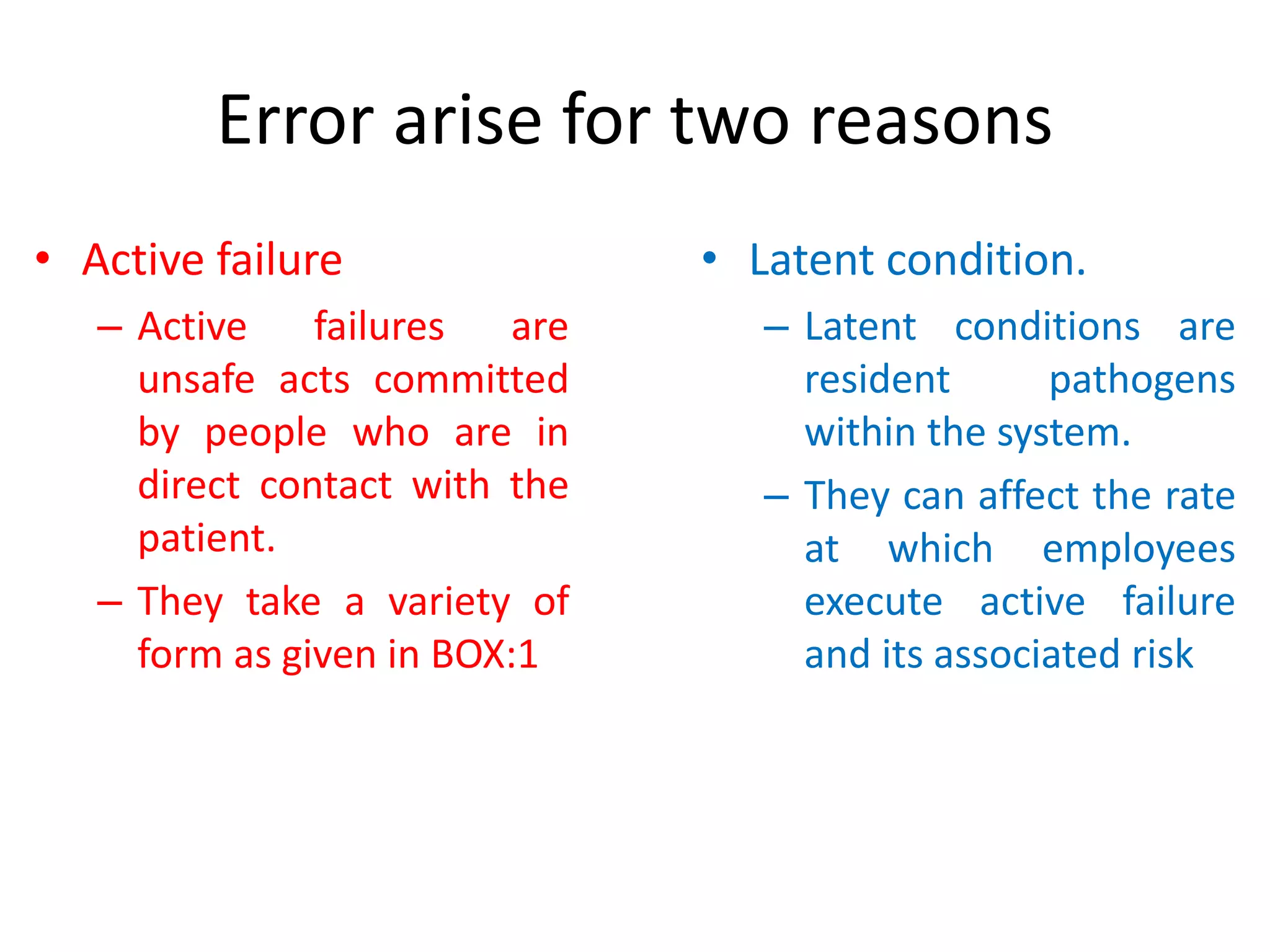
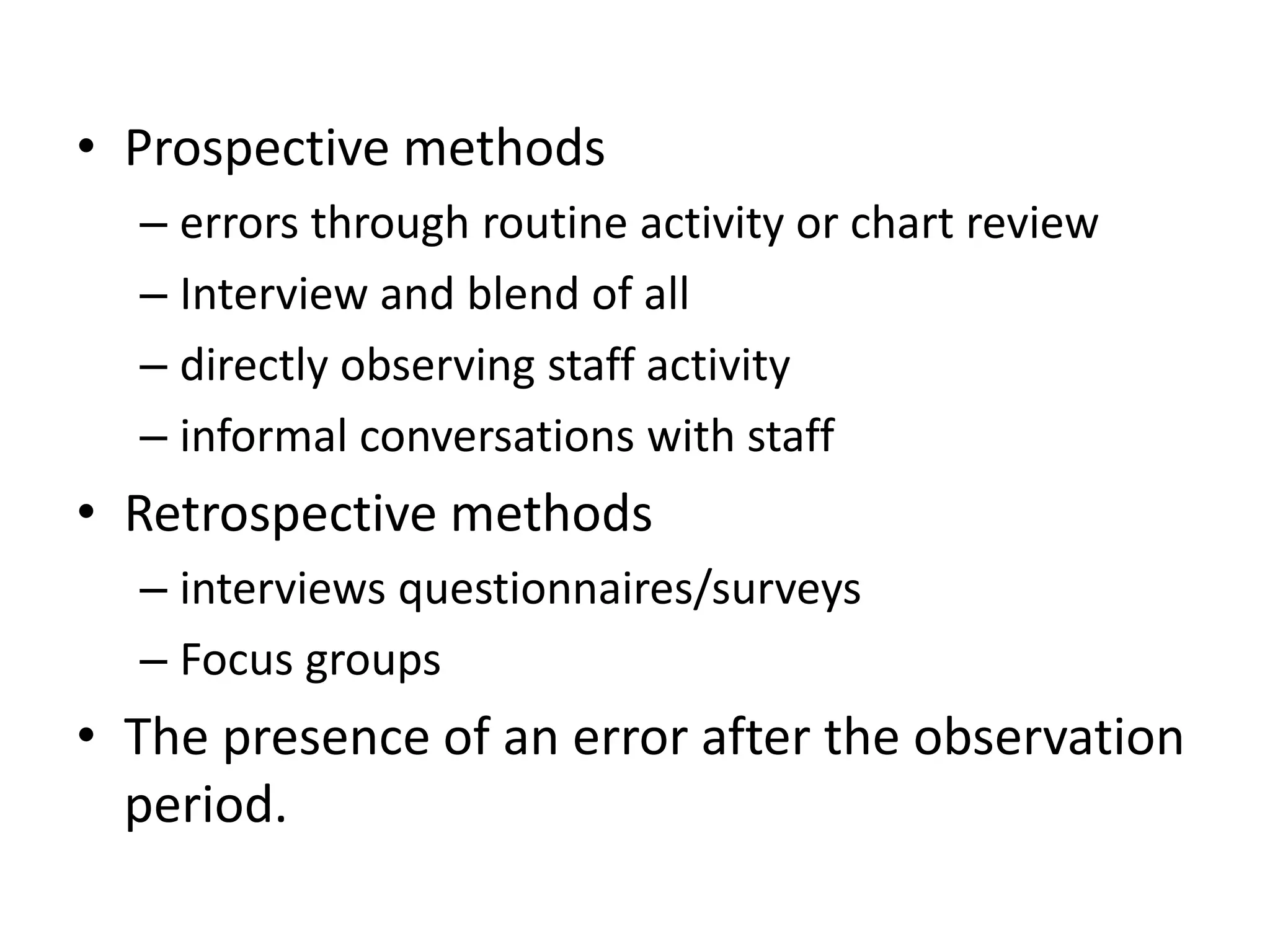
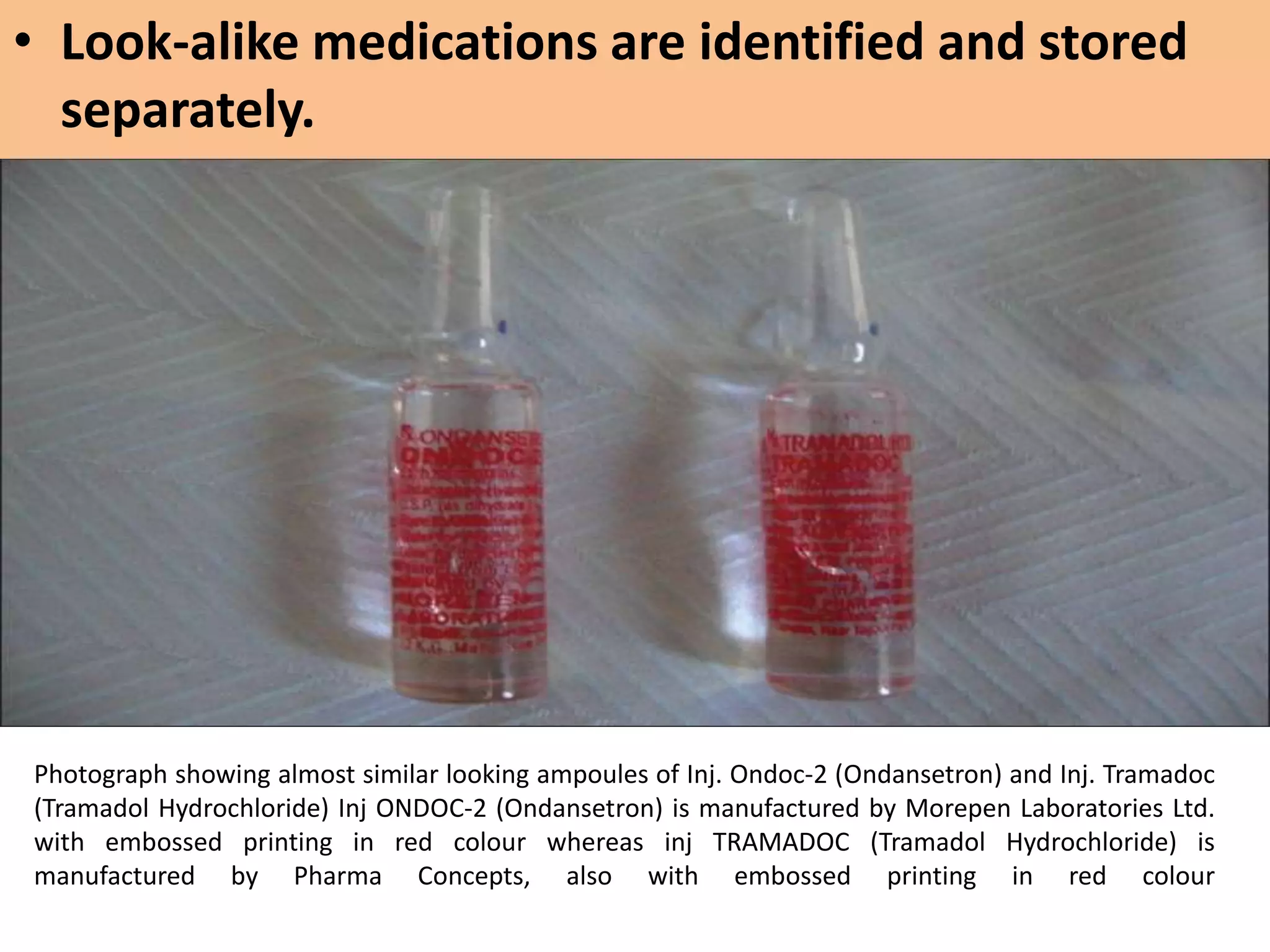
![Methodologies used to study
medication errors
• Direct observation method
– With some confirming the error once the medication
administration round had finished (n = 8)
– Observation with chart review
– Interviews [67] for prospective and retrospective error
identification.
• Prospective self-reporting methods such as
– Log books
– error (e.g. incident) reports
– drug administration view](https://image.slidesharecdn.com/medicationerror-140701054826-phpapp02/75/Medication-error-117-2048.jpg)